Robotic surgery for gastric cancer
Abstract
The number of robotic gastrectomy (RG) cases is increasing, especially in East Asia. The da Vinci Surgical System for RG allows surgeons to perform meticulous procedures using articulated devices and provides potential advantages over laparoscopic gastrectomy (LG). Meta-analyses including a large number of retrospective studies comparing RG and LG revealed only a limited advantage for RG over LG, such as lower blood loss, and the obvious disadvantage of longer operation times and higher medical cost. Specifically, a multicenter, prospective, single-arm study performed in Japan showed favorable short-term outcomes of RG over LG, while a non-randomized controlled trial in Korea showed similar postoperative complication rates for RG and LG, although the medical costs were significantly higher in RG. A well-designed randomized controlled trial is thus necessary to establish robust evidence comparing the two surgeries. In addition, further development of surgical robotics is expected for RG to be accepted more widely.
Keywords
Introduction
Gastric cancer is the third leading cause of cancer-related deaths and the fifth most common cancer worldwide[1]. Gastrectomy with radical lymphadenectomy is a mainstay of treatment on resectable gastric cancer; however, recent randomized controlled trials have demonstrated inferiorities of such expanded and invasive procedures[2-5]. In contrast, minimally invasive surgery including laparoscopic gastrectomy (LG) and robotic gastrectomy (RG) is attracting attention. LG was first introduced in 1991 in Japan[6], and since then, this procedure is used all over the world. The reported advantages of LG over radical open gastrectomy are faster recovery from the surgical stress, less bleeding, good cosmetic results, and shorter hospital stays[7-9]. Nevertheless, this procedure has several drawbacks such as two-dimensional surgical view and the motion restriction using linear forceps. Surgical robotics has introduced in 1990s having the potential to overcome those limitations and is spreading rapidly in the world.
In this review, we provide an historical outline of the development of surgical robotics, and describe the advantages and disadvantages of robot gastrectomy for gastric cancer compared to LG.
History of surgical robotics
The history and development of surgical robotics [Table 1] goes back to the 1950s, with the development of so-called “telepresence robotic arms”, although these were not intended for surgical applications, but rather for remotely controlled systems to handle hazardous substances or to perform tasks underwater or in space. In the 1980s, robotic arm development progressed rapidly with advances in computer technology, and in 1985, surgical robotics was first used in a clinical setting to perform a neurological biopsy[10]. A year later, researchers at the IBM Thomas J. Watson Research Center and University of California completed the development of ROBODOC, which became the first surgical robot approved by the USA Food and Drug Administration (FDA) for clinical use in humans[11]. In 1994, Computer Motion Inc. developed Automated Endoscopic System for Optimal Positioning (AESOP; Computer Motion Inc., USA) with the aim of solo-surgery using voice recognition to control the endoscope[12].
History of surgical robotics
| Year | Event |
|---|---|
| 1985 | Puma 200 was used for neurosurgical biopsy |
| 1986 | ROBODOC was used for artificial joint replacement |
| 1994 | AESOP (Computer Motion Inc.) released and approved by the FDA |
| 1998 | ZEUS (Computer Motion Inc.) released |
| 1999 | da Vinci Surgical System (Intuitive Surgical Inc.) released |
| 2000 | da Vinci Surgical System approved by the FDA |
| 2001 | First case of intercontinental telesurgery (US-France) |
| 2002 | Hashizume performed robot-assisted distal gastrectomy |
| 2003 | Merger of Intuitive Surgical Inc. and Computer Motion Inc. |
The US army also developed medical robotics for the use of telesurgery in the late 1980s with a master-slave manipulator system that was originally designed for battlefield surgery. This system was subsequently introduced into the clinical market as the da Vinci Surgical System (DVSS) by Intuitive Surgical Inc, and in 2000, DVSS became the first robot-assisted surgical system approved by the FDA for use in general laparoscopic surgery[13,14]. Computer Motion Inc. also developed ZEUS in 1998, adding a remote-control function to AESOP[15]. In the beginning, both systems were used only for cardiovascular surgery; however, they were gradually expanded to digestive surgery, urology, and gynecology. In 2001, ZEUS was used for the first case of telesurgery between New York and France to perform cholecystectomy[16]. This operation was called “Lindbergh operation” after the American aviator Charles Lindbergh who was the first person to fly solo across the Atlantic Ocean. The first RG [robotic distal gastrectomy (RDG)] for gastric cancer was reported in 2002 by Hashizume et al.[17] using DVSS.
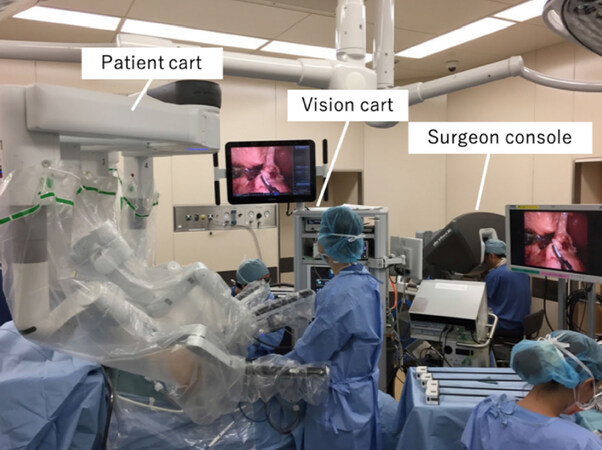
In 2003, Computer Motion Inc merged with Intuitive Surgical Inc., and since then DVSS has been the only FDA-approved surgery-assisting robot, building a near-monopoly. In September 2018, there were 4,814 installed DVSS units worldwide, including 3,110 in the United States, 821 in Europe, and 629 in Asia[18][Figure 1].
Current status of RG for gastric cancer
The most apparent advantage of RG over LG is that articulated devices are available in RG. In addition, the motion scaling and tremor suppression functions in RG enable more precise movement, which is believed to reduce tissue damage and blood loss. Another advantage of RG is a three-dimensional (3D) field of view that facilitates surgeons to recognize depth perception. Recently, 3D images also became available in LG; however, special glasses are necessary and the quality of imaging remains inferior to that in RG. Furthermore, the ergonomics-based surgery console used in RG can reduce the fatigue of operators. While the surgical devices for RG were limited at first, ultrasonically activated device (harmonic), vessel sealers, Endo Wrist staplers, and other instruments are now available.
Short-term outcomes
Retrospective studies
Numerous retrospective, case-control studies comparing RG and LG have been conducted, and several meta-analyses were performed using those studies [Table 2][19-26]. Shen et al.[19] conducted 8 studies with a total of 1,875 patients that showed approximately 40 mL lower blood loss in RG than LG; however, the operation time for RG was approximately 50 min longer. The duration of hospital stay, morbidity, and numbers of retrieved lymph nodes were comparable between RG and LG. Other meta-analysis indicated similar results, with the exception of a difference between RG over LG with morbidity. Guerra et al.[25] analyzed 8 studies, including 2026 patients, focusing on pancreatic complications. Pancreatic fistula occurred in 2.7% of patients receiving RG and 3.8% of patients receiving LG, for an odds ratio of 0.72. Although the difference was not statistically significant, the authors concluded that RG trended toward lower rates of postoperative pancreas-related events, despite more unfavorable baseline characteristics compared with LG.
Summary of the meta-analyses comparing RG and LG with respect to short term outcomes
| Author | Year | Country | Number of studies | Number of patients | Morbidity | Blood loss | Operation time | Retrieved LN | Hospital stay | Time to oral intake | Time to first flatus | Medical cost |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hyun et al.[26]* | 2013 | Korea | 9 | 7,200 | RG = LG | RG = LG | RG > LG | RG = LG | RG = LG | - | - | - |
| Shen et al.[19] | 2014 | China | 8 | 1,875 | RG = LG | RG < LG | RG > LG | RG = LG | RG = LG | - | - | - |
| Chuan et al.[20] | 2015 | China | 5 | 1,796 | RG = LG | RG < LG | RG > LG | RG = LG | RG = LG | - | - | - |
| Hu et al.[21] | 2016 | China | 12 | 3,580 | RG = LG | RG < LG | RG > LG | RG > LG | RG < LG | - | RG > LG | - |
| Wang et al.[23] | 2017 | China | 3 | 562 | RG = LG | RG = LG | RG > LG | RG = LG | RG = LG | - | - | - |
| Chen et al.[22] | 2017 | China | 19 | 5,953 | RG = LG | RG < LG | RG > LG | RG = LG | RG = LG | RG > LG | RG = LG | RG > LG |
| Guerra et al.[25] | 2018 | Italy | 8 | 2,026 | RG = LG** | - | RG > LG | RG > LG | RG = LG | - | - | - |
Prospective studies
Very limited prospective studies of RG have been conducted thus far. We conducted single-center early and late phase II studies in patients with cStage I gastric cancer to evaluate the safety of RG[27,28], involving 18 and 120 patients, respectively, in each study that found an incidence of intra-abdominal infectious complications of Clavien-Dindo classification grade ≥ II of 0% and 3.3%, respectively. Thus, the null hypotheses were rejected, and the studies concluded that RG can be safely used in cStage I gastric cancer.
In a prospective, multicenter, non-randomized, control study was conducted in Korea from May 2011 to December 2012 to compare the short-term surgical outcomes of RG (n = 223) and LG (n = 211)[29]. No significant difference was observed in the incidence of overall postoperative complications (RG 11.9%, LG 10.3%) and the mortality rate was 0% in both groups; however, the operation time was 40 min longer and the financial cost was 5,000 USD higher for RG than for LG. The authors concluded that RG was not superior to LG, and subsequent sub-group analysis showed a significantly lower amount of blood loss in RG when D2 lymph node dissection than that in LG[30].
A multicenter, prospective, single-arm study conducted in Japan evaluated the safety of RG in 330 patients with cStage I/II gastric cancer enrolled from October 2014 to January 2017, with the primary endpoint of postoperative complication[31]. The incidence of postoperative complications of Clavien-Dindo grade ≥ III was 2.45%, which was significantly lower than that in the historical control group (6.4%). Based on this result, RG for gastric cancer has been covered by national health insurance since April 2018 in Japan.
Long-term outcomes
A few retrospective case-control studies have been conducted to compare long-term outcomes between RG and LG in Japan and Korea[32-34]. In a study conducted in Japan, data from 84 patients who underwent RG and 437 patients who underwent LG around the same time were retrospectively analyzed; the 3-year overall survival rates were 86.9% and 88.8%, respectively, and did not differ to a statistically significant extent (P = 0.636)[33]. A study conducted in Korea using propensity score matching found 5-year overall survival rates of 93.2% in RG and 94.2% in LG; again the difference was not statistically significant (P = 0.4112)[34]. Although not prospective findings, these results indicate that the long-term outcomes of RG are not inferior to those of LG.
Learning curve
The learning curve for RG is reportedly shorter for experienced surgeons who had performed LG, estimated to total between 10 and 25 cases[35-39], although 40-60 cases is the estimated number needed to reach stabilization in LG[40,41]. Thus, although the 3D imaging and instrument flexibility of RG may help to make the learning curve less steep, the fact that an expert in LG performed the RG in many cases could have affected the results. In contrast, a recent study showed that stabilization of the operation time occurred after 25 cases, even for surgeons without prior LG experience, suggesting that prior LG experience is not necessarily required[42].
Nevertheless, robotic surgery requires surgeons to attain some extent of specialized training. Intuitive Surgical Inc. provides a training program and surgeons have to pass this program and be certificated as a Console Surgeon of DVSS to perform RG using DVSS. Interestingly, this training program targets surgeons from various fields and it is not sufficient to perform RG independently. Therefore, we have developed three-step educational program targeted at qualified surgeons [Table 3], who should perform more than 10 cases of RG including one or more cases of total or proximal gastrectomy[43]. A proctor scores the surgeon in accordance to the evaluation list, and when a high score is achieved, the surgeon will be allowed to perform RG independently.
Educational Program in Shizuoka Cancer Center
| Step | Target item | Purpose |
|---|---|---|
| 1 | Has taken the training courses led by Intuitive Surgical Inc. and acquired surgeon certification | Learn the basic operation of the da Vinci Surgical System and perform repetitive training of surgical techniques and surgical procedures |
| Perform at least 10 h of offsite training using the da Vinci Surgical System | Learn the smooth operation of the da Vinci Surgical System | |
| 2 | Under the guidance of the proctor, perform over 10 robotic gastrectomies (including total gastrectomies, cardia side gastrectomies)*1-4 Do not cause other organ damage requiring repair, arterial injuries requiring reconstruction, or other intraoperative complications requiring an open conversion | Gain experience in robotic gastrectomy |
| Perform one or more robotic total gastrectomies | Gain experience as a surgeon for robotic total gastrectomies to acquire esophagus jejunal anastomosis | |
| 3 | Achieve a rating of B or higher from the proctor in all items of the surgical evaluation on robotic distal gastrectomy | The proctor evaluates whether or not the target surgeon is appropriate as a robotic surgeon, according to unified standards |
Ergonomics
Robotic surgery provides surgeons with an ergonomically sound work environment because although LG is usually performed in the standing position, RG can be performed in a sitting position at an ergonomically designed surgeon console, which is expected to reduce operator fatigue. A survey study comprising 26 questions was performed to document the discomfort of robotic surgery compared with open and laparoscopic surgery, and to investigate the factors that affect the risk of physical symptoms, involving surgeons with various specialties and 1,215 who practiced all three approaches. This survey demonstrated that robot-assisted surgery was associated with the least physical discomfort and symptoms compared with open and laparoscopic surgery[44]. The breakdown of symptoms indicated that robotic surgery was less likely to lead to neck, back, hip, knee, ankle, foot, shoulder, elbow, and wrist pain than open or laparoscopic surgery, although the frequency of eye and finger pain was higher in robotic surgery. In another survey of 432 surgeons using robotic surgery in various fields, 56.1% complained of physical symptoms or discomfort, with the most frequent complaints being neck stiffness, finger pain, and eye fatigue[45]. Thus, although robotic surgery reduces the physical symptoms and discomfort of surgeons in comparison to open and laparoscopic surgery, more than 50% of surgeons have complained of a certain degree of physical stress, typically finger pain and eye strain.
Disadvantages of robotic compared to laparoscopic gastrectomy
The most critical disadvantage of RG is a lack of tactile perception, which can lead to incomplete ligature and tissue damage due to excessive stress. Visual information can compensate the lack of tactile perception; however, serious injury could still happen outside the field of view. Surgical robotics can potentially apply an unexpectedly strong force that never occurs in conventional surgery. Thus, even slight mishandling of the DVSS may lead to a fatal accident, even with a built-in system to prevent excessive compression to organs.
Requiring a long operation time is another disadvantage in RG. A retrospective study investigating factors contributing to prolongation of the operation time identified “junk time” as a cause of the prolongation[46]. In this study, the authors classified the overall operation time into two groups: the effective time (time required for actual surgical techniques such as port replacement, lymphadenectomy, and reconstruction) and the junk time (setup docking, and adjustment of surgical instruments). They found that junk time was significantly longer in RG, at 41.5 min, than in LG, though effective time was not statistically different between the groups. Although there was no difference in the number of instrument exchanges, the time required to exchange instruments was also significantly longer in RG than in LG. Additionally, the operation time was reduced by about 1 h when ultrasonically activated devices were used[47]. These studies suggest that a smarter and simpler system is needed for the setup and for instrument change, and development of new devices are warranted to reduce the operation time.
Future perspectives
A lack of robust evidence regarding RG use appears to be the most important future issue. Although RG has many theoretical advantages over LG, a definite and significant benefit of RG over LG has not been shown in a clinical setting due to the lack of randomized controlled trials (RCT). It cannot be denied that the high cost of RG affects the difficulty in conducting RCT, with some meta-analyses and a prospective study conducted in Korea indicating that RG is 4000-5000 USD more expensive than LG[22,29]. In Japan, RG has been covered by health insurance since April 2018; thus, patients can undergo RG without any extra cost. Thus, while the economic burden on medical institutions remains, the groundwork for RCT has been completed, and a well-designed RCT is needed to investigate the superiority of RG over LG.
Currently, several companies are developing surgical robots, with such market competition expected to decrease the price and further their use. Moreover, we anticipate the near future to bring development of new devices or miniaturization of existing surgical robots, together with innovative development, including concomitant use with 3D imaging[48], artificial intelligence, and virtual reality[49].
Conclusion
RG with DVSS facilitates meticulous surgical procedures with 3D imaging, instrument flexibility, tremor suppression, and improved ergonomics. Problems with RG remain including an unacceptable lack in tactile perception, longer operation times, and high medical costs. Moreover, although RG has theoretical advantages over LG, robust evidence is lacking. Well-designed, randomized controlled trials are therefore needed to establish stronger evidence and further develop the field of surgical robotics.
Declarations
Authors’ contributionsDesigned the study, reviewed literature, and wrote the manuscript: Makuuchi R
Critical revision of the manuscript and approval of the final version: Kamiya S, Tanizawa Y, Bando E
Writing the manuscript, drafting and critical revision and editing, and approval of the final version: Terashima M
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2019.
REFERENCES
1. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87-108.
2. Sano T, Sasako M, Mizusawa J, Yamamoto S, Katai H, et al. Randomized Controlled Trial to Evaluate Splenectomy in Total Gastrectomy for Proximal Gastric Carcinoma. Ann Surg 2017;265:277-83.
3. Sasako M, Sano T, Yamamoto S, Kurokawa Y, Nashimoto A, et al. D2 lymphadenectomy alone or with para-aortic nodal dissection for gastric cancer. N Engl J Med 2008;359:453-62.
4. Sasako M, Sano T, Yamamoto S, Sairenji M, Arai K, et al. Left thoracoabdominal approach versus abdominal-transhiatal approach for gastric cancer of the cardia or subcardia: a randomised controlled trial. Lancet Oncol 2006;7:644-51.
5. Terashima M, Doki Y, Kurokawa Y, Mizusawa J, Katai H, et al. Primary results of a phase III trial to evaluate bursectomy for patients with subserosal/serosal gastric cancer (JCOG1001). J Clin Oncol 2017;35:5.
6. Kitano S, Iso Y, Moriyama M, Sugimachi K. Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 1994;4:146-8.
7. Kodera Y, Fujiwara M, Ohashi N, Nakayama G, Koike M, et al. Laparoscopic surgery for gastric cancer: a collective review with meta-analysis of randomized trials. J Am Coll Surg 2010;211:677-86.
8. Katai H, Mizusawa J, Katayama H, Takagi M, Yoshikawa T, et al. Short-term surgical outcomes from a phase III study of laparoscopy-assisted versus open distal gastrectomy with nodal dissection for clinical stage IA/IB gastric cancer: Japan Clinical Oncology Group Study JCOG0912. Gastric Cancer 2017;20:699-708.
9. Katai H, Mizusawa J, Katayama H, Kunisaki C, Sakuramoto S, et al. Single-arm confirmatory trial of laparoscopy assisted total or proximal gastrectomy with nodal dissection for clinical stage I gastric cancer: Japan Clinical Oncology Group study JCOG1401. J Clin Oncol 2018;36:4028.
10. Kwoh YS, Hou J, Jonckheere EA, Hayati S. A robot with improved absolute positioning accuracy for CT guided stereotactic brain surgery. IEEE Trans Biomed Eng 1988;35:153-60.
11. Paul HA, Bargar WL, Mittlestadt B, Musits B, Taylor RH, et al. Development of a surgical robot for cementless total hip arthroplasty. Clin Orthop Relat Res 1992:57-66.
13. Falk V, Diegeler A, Walther T, Banusch J, Brucerius J, et al. Total endoscopic computer enhanced coronary artery bypass grafting. Eur J Cardiothorac Surg 2000;17:38-45.
14. Cadiere GB, Himpens J, Germay O, Izizaw R, Degueldre M, et al. Feasibility of robotic laparoscopic surgery: 146 cases. World J Surg 2001;25:1467-77.
15. Reichenspurner H, Damiano RJ, Mack M, Boehm DH, Gulbins H, et al. Use of the voice-controlled and computer-assisted surgical system ZEUS for endoscopic coronary artery bypass grafting. J Thorac Cardiovasc Surg 1999;118:11-6.
16. Marescaux J, Leroy J, Gagner M, Rubino F, Mutter D, et al. Transatlantic robot-assisted telesurgery. Nature 2001;413:379-80.
17. Hashizume M, Shimada M, Tomikawa M, Ikeda Y, Takahashi I, et al. Early experiences of endoscopic procedures in general surgery assisted by a computer-enhanced surgical system. Surg Endosc 2002;16:1187-91.
18. Surgical I. Investors Overview: Featured Documents; Investor Presentation Q4 2018. Available from: https://isrg.gcs-web.com/. [Last accessed on 9 Apr 2019].
19. Shen WS, Xi HQ, Chen L, Wei B. A meta-analysis of robotic versus laparos copic gastrectomy for gastric cancer. Surg Endosc 2014;28:2795-802.
20. Chuan L, Yan S, Pei-Wu Y. Meta-analysis of the short-term outcomes of robotic-assisted compared to laparoscopic gastrectomy. Minim Invasive Ther Allied Technol 2015;24:127-34.
21. Hu LD, Li XF, Wang XY, Guo TK. Robotic versus laparoscopic gastrectomy for gastric carcinoma: a meta-analysis of efficacy and safety. Asian Pac J Cancer Prev 2016;17:4327-33.
22. Chen K, Pan Y, Zhang B, Maher H, Wang XF, et al. Robotic versus laparoscopic gastrectomy for gastric cancer: a systematic review and updated meta-analysis. BMC Surg 2017;17:93.
23. Wang Y, Zhao X, Song Y, Cai A, Xi H, et al. A systematic review and meta-analysis of robot-assisted versus laparoscopically assisted gastrectomy for gastric cancer. Medicine (Baltimore) 2017;96:e8797.
24. Huang KH, Lan YT, Fang WL, Chen JH, Lo SS, et al. Comparison of the operative outcomes and learning curves between laparoscopic and robotic gastrectomy for gastric cancer. PLoS One 2014;9:e111499.
25. Guerra F, Giuliani G, Formisano G, Bianchi PP, Patriti A, et al. Pancreatic complications after conventional laparoscopic radical gastrectomy versus robotic radical gastrectomy: systematic review and meta-analysis. J Laparoendosc Adv Surg Tech A 2018;28:1207-15.
26. Hyun MH, Lee CH, Kwon YJ, Cho SI, Jang YJ, et al. Robot versus laparoscopic gastrectomy for cancer by an experienced surgeon: comparisons of surgery, complications, and surgical stress. Ann Surg Oncol 2013;20:1258-65.
27. Tokunaga M, Sugisawa N, Kondo J, Tanizawa Y, Bando E, et al. Early phase II study of robot-assisted distal gastrectomy with nodal dissection for clinical stage IA gastric cancer. Gastric Cancer 2014;17:542-7.
28. Tokunaga M, Makuuchi R, Miki Y, Tanizawa Y, Bando E, et al. Late phase II study of robot-assisted gastrectomy with nodal dissection for clinical stage I gastric cancer. Surg Endosc 2016;30:3362-7.
29. Kim HI, Han SU, Yang HK, Kim YW, Lee HJ, et al. Multicenter prospective comparative study of robotic versus laparoscopic gastrectomy for gastric adenocarcinoma. Ann Surg 2016;263:103-9.
30. Park JM, Kim HI, Han SU, Yang HK, Kim YW, et al. Who may benefit from robotic gastrectomy? A subgroup analysis of multicenter prospective comparative study data on robotic versus laparoscopic gastrectomy. Eur J Surg Oncol 2016;42:1944-9.
31. Uyama I, Suda K, Nakauchi M, Kinoshita T, Noshiro H, et al. Clinical advantages of robotic gastrectomy for clinical stage I/II gastric cancer: a multi-institutional prospective single-arm study. Gastric Cancer 2019;22:377-85.
32. Son T, Lee JH, Kim YM, Kim HI, Noh SH, et al. Robotic spleen-preserving total gastrectomy for gastric cancer: comparison with conventional laparoscopic procedure. Surg Endosc 2014;28:2606-15.
33. Nakauchi M, Suda K, Susumu S, Kadoya S, Inaba K, et al. Comparison of the long-term outcomes of robotic radical gastrectomy for gastric cancer and conventional laparoscopic approach: a single institutional retrospective cohort study. Surg Endosc 2016;30:5444-52.
34. Obama K, Kim YM, Kang DR, Son T, Kim HI, et al. Long-term oncologic outcomes of robotic gastrectomy for gastric cancer compared with laparoscopic gastrectomy. Gastric Cancer 2018;21:285-95.
35. D’Annibale A, Pende V, Pernazza G, Monsellato I, Mazzocchi P, et al. Full robotic gastrectomy with extended (D2) lymphadenectomy for gastric cancer: surgical technique and preliminary results. J Surg Res 2011;166:e113-20.
36. Eom BW, Yoon HM, Ryu KW, Lee JH, Cho SJ, et al. Comparison of surgical performance and short-term clinical outcomes between laparoscopic and robotic surgery in distal gastric cancer. Eur J Surg Oncol 2012;38:57-63.
37. Huang KH, Lan YT, Fang WL, Chen JH, Lo SS, et al. Initial experience of robotic gastrectomy and comparison with open and laparoscopic gastrectomy for gastric cancer. J Gastrointest Surg 2012;16:1303-10.
38. Kang BH, Xuan Y, Hur H, Ahn CW, Cho YK, et al. Comparison of surgical outcomes between robotic and laparoscopic gastrectomy for gastric cancer: the learning curve of robotic surgery. J Gastric Cancer 2012;12:156-63.
39. Uyama I, Kanaya S, Ishida Y, Inaba K, Suda K, et al. Novel integrated robotic approach for suprapancreatic D2 nodal dissection for treating gastric cancer: technique and initial experience. World J Surg 2012;36:331-7.
40. Kim MC, Jung GJ, Kim HH. Learning curve of laparoscopy-assisted distal gastrectomy with systemic lymphadenectomy for early gastric cancer. World J Gastroenterol 2005;11:7508-11.
41. Jin SH, Kim DY, Kim H, Jeong IH, Kim MW, et al. Multidimensional learning curve in laparoscopy-assisted gastrectomy for early gastric cancer. Surg Endosc 2007;21:28-33.
42. An JY, Kim SM, Ahn S, Choi MG, Lee JH, et al. Successful robotic gastrectomy does not require extensive laparoscopic experience. J Gastric Cancer 2018;18:90-8.
43. Terashima M. Educational program on robotic gastrectomy in shizuoka cancer center. Available from: https://www.scchr.jp/en/wp-content/uploads/sites/18/2017/02/Educational-Program-on-Robotic-Gastrectomy.pdf. [Last accessed on 9 Apr 2019].
44. Plerhoples TA, Hernandez-Boussard T, Wren SM. The aching surgeon: a survey of physical discomfort and symptoms following open, laparoscopic, and robotic surgery. J Robot Surg 2012;6:65-72.
45. Lee GI, Lee MR, Green I, Allaf M, Marohn MR. Surgeons’ physical discomfort and symptoms during robotic surgery: a comprehensive ergonomic survey study. Surg Endosc 2017;31:1697-706.
46. Liu H, Kinoshita T, Tonouchi A, Kaito A, Tokunaga M. What are the reasons for a longer operation time in robotic gastrectomy than in laparoscopic gastrectomy for stomach cancer? Surg Endosc 2019;33:192-8.
47. Hikage M, Tokunaga M, Makuuchi R, Tanizawa Y, Bando E, et al. Impact of an Ultrasonically Activated Device in Robot-Assisted Distal Gastrectomy. Innovations (Phila) 2017;12:453-8.
48. Furukawa J, Miyake H, Tanaka K, Sugimoto M, Fujisawa M. Console-integrated real-time three-dimensional image overlay navigation for robot-assisted partial nephrectomy with selective arterial clamping: early single-centre experience with 17 cases. Int J Med Robot 2014;10:385-90.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Makuuchi R, Kamiya S, Tanizawa Y, Bando E, Terashima M. Robotic surgery for gastric cancer. Mini-invasive Surg 2019;3:11. http://dx.doi.org/10.20517/2574-1225.2019.03
AMA Style
Makuuchi R, Kamiya S, Tanizawa Y, Bando E, Terashima M. Robotic surgery for gastric cancer. Mini-invasive Surgery. 2019; 3: 11. http://dx.doi.org/10.20517/2574-1225.2019.03
Chicago/Turabian Style
Makuuchi, Rie, Satoshi Kamiya, Yutaka Tanizawa, Etsuro Bando, Masanori Terashima. 2019. "Robotic surgery for gastric cancer" Mini-invasive Surgery. 3: 11. http://dx.doi.org/10.20517/2574-1225.2019.03
ACS Style
Makuuchi, R.; Kamiya S.; Tanizawa Y.; Bando E.; Terashima M. Robotic surgery for gastric cancer. Mini-invasive. Surg. 2019, 3, 11. http://dx.doi.org/10.20517/2574-1225.2019.03
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 20 clicks
Cite This Article 20 clicks












Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.