Technique of robotic lobectomy III: control of major vascular injury, the 5 “P”'s
Abstract
Robotic Lobectomy has been evolving over the past decade and has been shown to be an oncologically efficacious procedure. Although robotic lobectomy is performed more frequently in centers around the world, it accounts for a small percentage of all lobectomies. One of the major causes of reluctance to adopt robotic lobectomy and segmentectomy procedures by surgeons is the fear of bleeding complications, as well as the lack of a standardized reproducible approach to these potentially catastrophic events. This paper outlines a proven strategy for control of bleeding complications during robotic lobectomy and segmentectomy procedures: the 5 “P”’s of Prevention, Preparedness, Poise, Pressure, and Proximal Control.
Keywords
Introduction
Although robotic lobectomy is performed more frequently in centers around the world, it accounts for a small percentage of all lobectomies. One of the determinants for the lower level of adoption of the robotic lobectomy and segmentectomy procedures is concern about catastrophic bleeding complications, as well as a reproducible strategy for the control of bleeding.
The overall incidence of major vascular injury during elective robotic thoracic operations was reported to be 1.2% (16 of 1,304 operations) by Cerfolio et al.[1]. These authors reported the incidence of major vascular injury during robotic lobectomy as 2.6% and for robotic segmentectomy as 1.5%. Novellis et al.[2] reported an overall conversion rate of 6.2% (21/338) for major robotic lung resections, of which 1.1% (4/338) were due to bleeding. Other authors have reported overall conversion rates of 1.5%-9% with pulmonary artery or pulmonary vein injury resulting in conversion in 0.5%-2.6%[3-7]. In a retrospective multi-institutional study of 1,810 patients who underwent robotic anatomic pulmonary resections, Cao et al.[4] reported intraoperative catastrophic events in 1.9% of patients Catastrophic events were associated with higher proportion of patients who underwent preoperative radiotherapy, higher perioperative mortality, longer operative times, and higher estimated blood loss. In this study, intraoperative hemorrhage from the pulmonary artery was the most common catastrophic event.
Gharagozloo et al.[3] reported their experience with 638 consecutive robotic lobectomies for early stage lung cancer. Conversion to a thoracotomy occurred in 11 (1.7%) patients. Six of eleven (54%) conversions were for bleeding (0.9% of robotic lobectomies).
The most common intraoperative bleeding complication during robotic lung resection is from an injury to the pulmonary artery. Most commonly, pulmonary artery injury occurs during dissection of the artery[4]. These injuries are easier to see as they occur directly at the point of dissection. Injury to the pulmonary artery can also occur at the time of encirclement of the artery branch and passage of the stapling device[5,6]. In these instances, the pulmonary artery is usually torn at the branch point resulting in a more central injury. Most commonly, a central pulmonary artery injury occurs during left upper lobectomy and is associated with dissection, isolation, and division of the truncus branch. The risk factors for pulmonary artery injury with robotic lung resection are similar to open or conventional video-assisted (VATS) procedures. The risk of pulmonary artery injury is increased in patients who have received induction chemo- and/or radiation therapy, have larger tumors, and in the presence of calcified lymph nodes[6-8].
Pulmonary vein injury is much less common than pulmonary arterial injury[4]. Pulmonary vein injuries can be more easily repaired using minimally invasive techniques such as stapling or over sewing. The most important technical aspect of managing a pulmonary vein injury is to prevent air embolism by resisting vigorous suction at the bleeding point. Control of the pulmonary vein bleeding by “pressure” is preferred and is similar to what is outlined for the artery below.
This paper outlines a proven strategy for control of bleeding complications during robotic lung resections.
Strategy for the Control of Major Vascular Injury: Cerfolio et al.[1] described the 4 “P”’s as the technique for the control of major vascular injury: Poise, Pressure, Preparedness, and Proximal Control. Preparedness can be further expanded to Prevention of the injury and Preparedness of the team to respond to the catastrophic event.
The 5 “P”’s
Prevention
First and foremost is Prevention. Prevention of major vascular injury dictates a different approach to the dissection of the vascular structures during robotic lung resection. Unlike the technique of open and VATS lobectomy where the artery branches are dissected and divided in a sequential manner, robotic lung surgery requires a wider dissection of the mediastinum, the proximal and distal portions of the artery and vein. The strategy of robotic lung resection starts with a wide mediastinal nodal dissection with identification of the proximal broncho-vascular structures. This is followed by dissection of the smaller vascular branches. As a general rule, the dissection of the smaller vascular branch should only be undertaken after the more proximal portion of the artery or vein has been fully dissected. This strategy results in less tension on the branch points, ready access to the proximal portion of the artery or vein in the case of injury, and a more controlled approach to the bleeding complication, which, in turns, increases the odds of mitigation of bleeding without resorting to conversion to a thoracotomy. Prevention of major vascular injury requires complete and methodical dissection of the perivascular structures, as outlined in Technique of Robotic Lobectomy I and II. The completion of the mediastinal nodal dissection allows for mobilization of the bronchial and vascular structures. Dissection and removal of perivascular N1 nodes allows for full visualization of the PA branches and allows for a safer approach to the isolation and division of the vessel. The use of vessel loops for elevation of the vascular branch and the use of staplers with guide catheters further decreases the chance of vascular injury. As a rule, the branch of the pulmonary artery and the proximal portion of the artery which gives rise to the branch should be completely dissected before any attempt is made to encircle the branch. Decreasing tension on the branch point is an excellent technique for avoiding injury to the artery. In general, greater dissection leads to safer control of the pulmonary artery branches and prevention of catastrophic bleeding. Furthermore, following these principles facilitates proximal control and control of bleeding in the event of injury to the pulmonary artery. In our view, all the steps of robotic lobectomy should be designed to build a foundation of safety for prevention of vascular injury. The “P” for prevention is the most important of the 5 “P”’s.
Preparedness
Anesthesia and the surgical team need to prepare by running drills such that each team member is totally ready for their function in the event of vascular injury. This requires a dedicated anesthesia and nursing team. Thoracotomy trays must be in the room, and possibly opened and counted depending on the experience of the surgeon. Blood needs to be available, dictating the need to routinely type and cross match blood for the patients who undergo robotic lobectomy and segmentectomy.
Poise
Poise is the first and most critical aspect of the response to a catastrophic injury. The primary surgeon must remain as relaxed as possible in order to create a calm and methodical approach to the problem. The primary surgeon needs to impart an attitude of confidence and calmness to all members of the surgical and anesthesia teams. This is only possible when there is a specific anesthesia and OR team, and if the team has prepared for the emergency by running regular disaster readiness drills.
Pressure
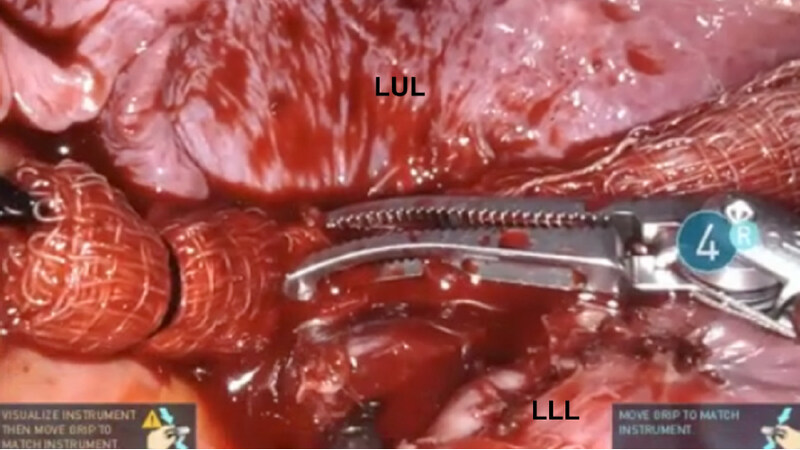
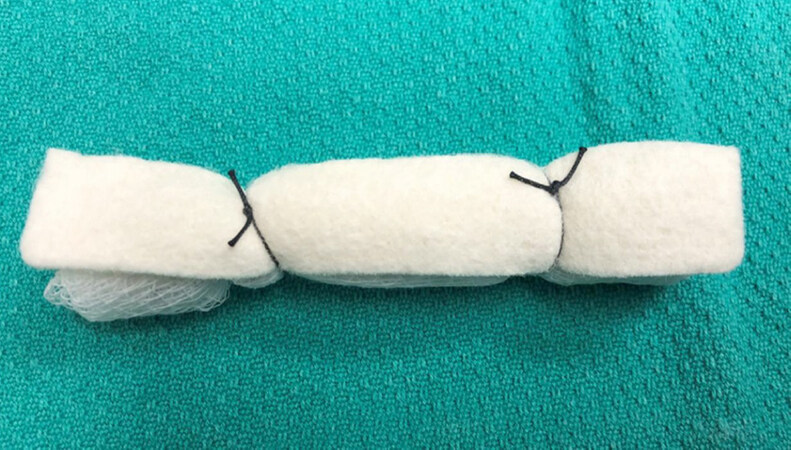
By virtue of being a low pressure and high flow vessel, pulmonary artery bleeding can be controlled with pressure. Attempts at grabbing the artery should be discouraged as this maneuver which works best for high pressure vessels will tend to enlarge the tear. The best approach is to have a tightly rolled sponge in the field. In the event of bleeding, the rolled sponge is placed over the bleeding point with the left robotic instrument (usually Cadiere forceps) and pressure is maintained [Figure 1]. Next, the assistant introduces a tightly rolled sponge which is covered with “EVARREST” fibrin sealant patch (Ethicon, Inc. Somerville, NJ, USA) [Figures 2 and 3]. The patch attached to a tightly rolled sponge is grasped by the right robotic instrument (usually a curved bipolar). In a swift motion, the sponge in the left hand is removed and replaced with the sponge carrying the EVERREST patch [Figure 4]. The patch is held over the bleeding point for exactly 3 min. Following this, the patch should be left in place and the fourth arm should be used to continue pressure on the sponge/patch composite. The tendency to assess the state of the tear should be absolutely avoided. The patch should be left in place until proximal control is obtained.
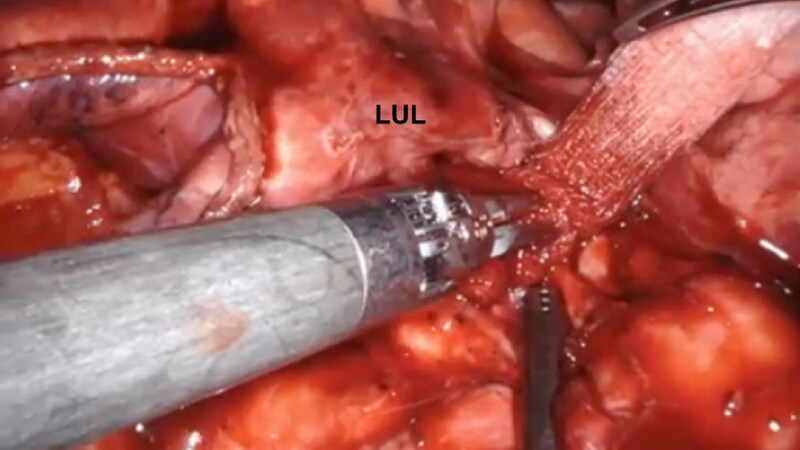
Figure 1. Injury to the superior segmental pulmonary artery, during left lower lobectomy. A rolled sponge which is always placed in the proximity of the dissection is used to control the bleeding using the right robotic arm. LUL: left upper lobe; LLL: left lower lobe
Figure 2. Injury to the superior segmental pulmonary artery, during left lower lobectomy. A rolled sponge which is always placed in the proximity of the dissection is used to control the bleeding using the right robotic arm. The blood is removed by the assistant using suction and the sponge is more accurately placed over the injury. LUL: left upper lobe; LLL: left lower lobe
Figure 4. At the first sign of a bleeding complication, the EVERREST Patch is prepared. The strip of EVERREST is tied onto the tightly rolled sponge and introduced through the accessory port by the assistant
Pulmonary vein injury usually occurs during dissection and encirclement maneuvers. Most commonly, the upper lobe veins are injured. Usually, the injury is on the underside of the vein. In the case of pulmonary vein injury, suction of blood should be avoided as this may lead to air (CO
It is important to emphasize that the experience of the surgeon with robotic procedures should dictate the next steps following control of the bleeding. For the less experienced surgeons, the safest strategy is to maintain pressure control of the bleeding and calmly convert to a thoracotomy. Using the accessory port, the assistant can introduce a long metal “Yankauer” suction to place direct pressure on the rolled sponge and/or sponge/EVERREST patch. With pressure control of the bleeding point, the robot arms are removed, and the camera is disconnected from the robot arm and introduced freely through the camera port in order to maintain full visualization of the pleural space and to confirm the control of the bleeding under direct vision. The robot is then moved away from the operating table, and the table is unlocked and turned to the normal position for a thoracotomy. The second assistant is tasked with pressure control of the bleeding point while a scrub nurse holds the camera for visual confirmation. Although some surgeons prefer to disconnect the left arm from the robot cart and use it for pressure control, if a second assistant is available, we prefer the suction pressure technique. The posterolateral thoracotomy is performed calmly and under control. The chest is entered through the 5th intercostal space directly over the oblique fissure in order to have full access to the hilum and the proximal pulmonary artery. After the chest is open, the Yankauer suction is replaced with a conventional kittner carrying a rolled sponge and the pressure control is maintained by the second assistant while the surgeon and the first assistant gain proximal control.
Surgeons with greater experience can obtain proximal control and repair the vascular injury by robotic or endoscopic techniques. However, it must be emphasized that conversion to a thoracotomy should be seen as the safest technique and conversion should be performed in a timely fashion and not as a last resort.
Proximal control
Once the vessel is hemostatic, the surgeon should obtain proximal control by passing a vessel loop around the pulmonary artery or vein proximally, double loop around it, and gently pull up to completely stop its blood flow. At this point, the patch sponge composite should be removed. The injury can be seen because the blood flow is stopped, and it can be sewn using 4-0 nonabsorbable suture or stapled if there is room proximally.
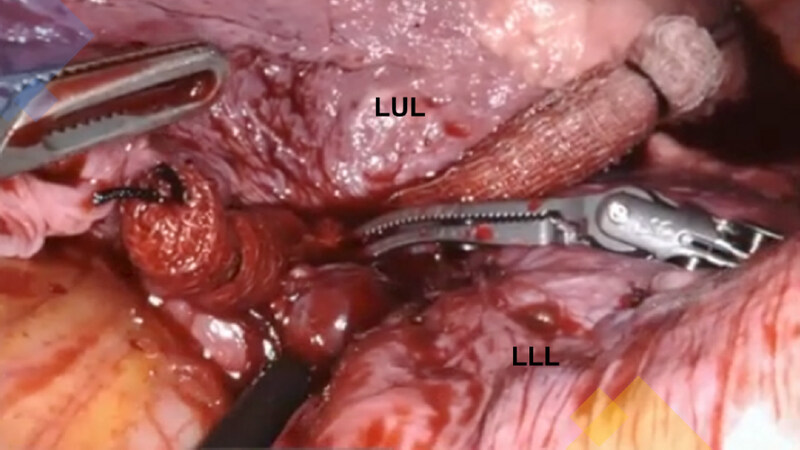
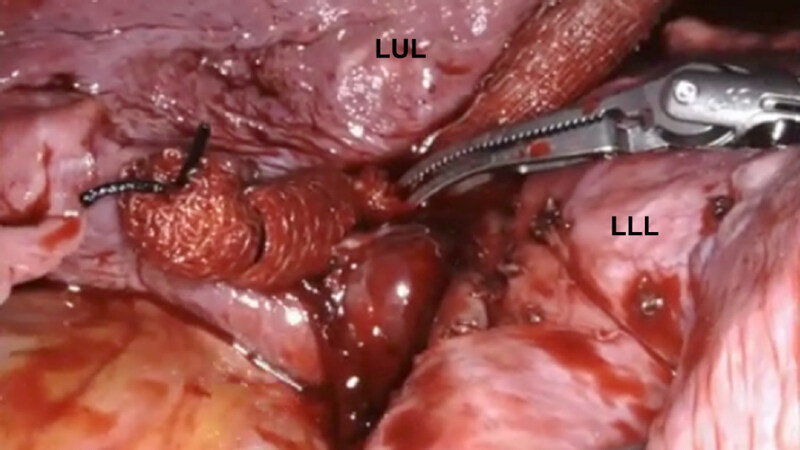
In our experience, pulmonary artery injury should be categorized into two groups: Group I, injury to pulmonary artery branch; and Group II, injury to a central portion of the pulmonary artery. In Group I, the bleeding is usually controlled using the EVERREST technique. In these patients, once the bleeding is controlled, proximal pulmonary artery control is obtained, and bleeding is mitigated using robotic techniques. The most common scenario is to staple the more proximal portion of the pulmonary artery branch [Figures 5 and 6].
Figure 5. The EVERREST patch is placed over the injury and held in place for 3 min by the clock. LUL: left upper lobe; LLL: left lower lobe
Figure 6. The EVERREST patch is left in place while obtaining proximal control. LUL: left upper lobe; LLL: left lower lobe
In Group II, the injury to the pulmonary artery is more central and requires control of the main pulmonary artery. This group is illustrated by injury to the proximal pulmonary artery during a robotic upper lobectomy procedure. In this group, the EVERREST technique allows for better but not perfect control of the bleeding. In these patients, the pressure needs to be maintained, the robotic procedure needs to be converted to a thoracotomy, and the vascular injury needs to be repaired in a safe manner.
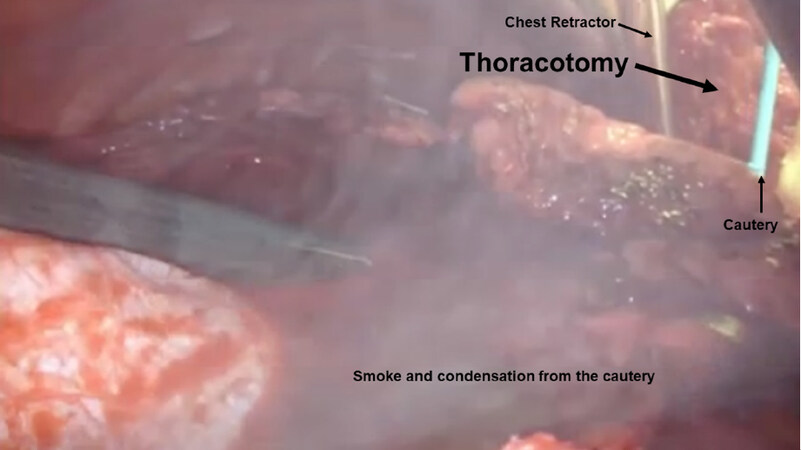
If conversion to thoracotomy is chosen, the robotic instruments need to be completely removed, the robot undocked and moved completely away from the operative field, and the bleeding stopped by the sponges and the pressure maintained on the sponge by an external suction manned by the assistant. Robotic instruments should not be used to hold pressure. In our view, it is best to avoid leaving one arm of the robot in to compress a vessel. It is critical to completely remove the robot from the operative field. If a vessel is still bleeding, pressure needs to be held by means of a nonrobotic instrument through the access port by a bedside assistant while the chest is safely and calmly opened [Figures 7-11].
Figure 7. Injury to the proximal pulmonary artery during robotic left upper lobectomy. The rolled sponge with EVERREST patch is used to control the bleeding in preparation for a thoracotomy. LUL: left upper lobe
Figure 8. Closeup view of injury to the proximal pulmonary artery during robotic left upper lobectomy. The rolled sponge with EVERREST patch is used to control the bleeding in preparation for a thoracotomy
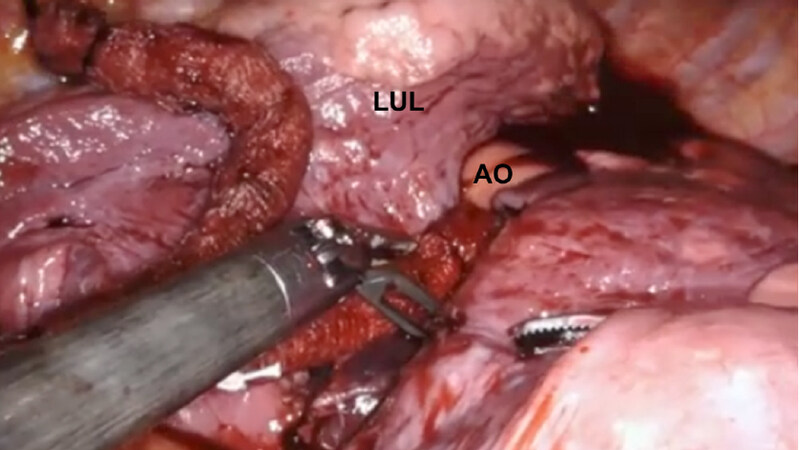
Figure 9. Injury to the proximal pulmonary artery during robotic left upper lobectomy. Due to the inability to obtain direction compression of the injury, the rolled sponge with EVERREST patch is not sufficient for controlling the bleeding. It is used to control the bleeding in preparation for a thoracotomy. LUL: left upper lobe; AO: aortic arch
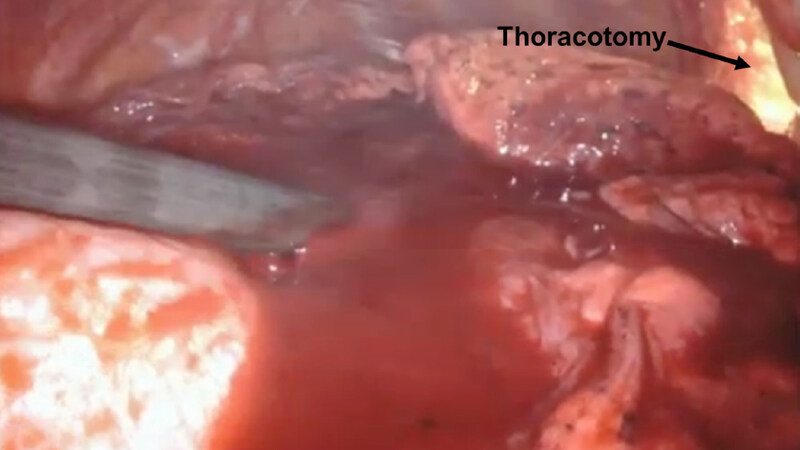
Figure 10. Injury to the proximal pulmonary artery during robotic left upper lobectomy. The robotic arms are removed. Bleeding is controlled by pressure on the EVERREST patch. The assistant introduces a suction introduced through the accessory port, while the surgical team converts to a thoracotomy
Figure 11. Injury to the proximal pulmonary artery during robotic left upper lobectomy. Thoracotomy is completed in preparation of proximal control and safe repair of the pulmonary artery injury
With greater experience, the minimally invasive technique can be used to control pulmonary artery bleeding. However, until greater experience is gained, and even then, under certain circumstances, an orderly conversion to a thoracotomy should remain the procedure of choice.
Conclusion
Intraoperative bleeding complications and catastrophes during pulmonary resection are rare. In fact, due to the uncommon nature of these complications, the surgical team is usually unprepared to manage the catastrophic bleeding and therefore these complications can result in significant consequences for the patient. Robotic surgical teams must have a well-rehearsed reproducible “fire drill” plan so that the team members understand their roles during these uncommon yet potentially catastrophic events. The application of the 5 “P”’s to robotic lung resection will increase patent safety and surgeon adoption of these procedures.
Declarations
Authors’ contributionsCollected the data, designed and performed the procedures, and composed the manuscript: Gharagozloo F, Meyer M
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestBoth authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2020.
REFERENCES
1. Cerfolio RJ, Bess KM, Wei B, Minnich DJ. Incidence, results, and our current intraoperative technique to control major vascular injuries during minimally invasive robotic thoracic surgery. Ann Thorac Surg 2016;102:394-9.
2. Novellis P, Jadoon M, Cariboni U, Bottoni E, Pardolesi A, et al. Management of robotic bleeding complications. Ann Cardiothorac Surg 2019;8:292-5.
3. Gharagozloo F, Meyer M, Tempesta B. Robotic lobectomy: experience with 638 consecutive cases. Surg Technol Int 2020;36:251-6.
4. Cao C, Cerfolio RJ, Louie BE, Melfi F, Beronesi G, et al. Incidence, management, and outcomes of intraoperative catastrophes during robotic pulmonary resection. Ann Thorac Surg 2019;108:1498-504.
5. Yang HX, Woo KM, Sima CS, Bains MS, Adusumilli PS, et al. Long-term survival based on the surgical approach to lobectomy for clinical stage I nonsmall cell lung cancer: comparison of robotic, video-assisted thoracic surgery, and thoracotomy lobectomy. Ann Surg 2017;265:431-7.
6. Louie BE. Catastrophes and complicated intraoperative events during robotic lung resection. J Vis Surg 2017;3:52.
7. Mei J, Pu Q, Liao H, Ma L, Zhu Y, et al. A novel method for troubleshooting vascular injury during anatomic thoracoscopic pulmonary resection without conversion to thoracotomy. Surg Endosc 2013;27:530-7.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Gharagozloo F, Meyer M. Technique of robotic lobectomy III: control of major vascular injury, the 5 “P”'s. Mini-invasive Surg 2020;4:57. http://dx.doi.org/10.20517/2574-1225.2020.44
AMA Style
Gharagozloo F, Meyer M. Technique of robotic lobectomy III: control of major vascular injury, the 5 “P”'s. Mini-invasive Surgery. 2020; 4: 57. http://dx.doi.org/10.20517/2574-1225.2020.44
Chicago/Turabian Style
Gharagozloo, Farid, Mark Meyer. 2020. "Technique of robotic lobectomy III: control of major vascular injury, the 5 “P”'s" Mini-invasive Surgery. 4: 57. http://dx.doi.org/10.20517/2574-1225.2020.44
ACS Style
Gharagozloo, F.; Meyer M. Technique of robotic lobectomy III: control of major vascular injury, the 5 “P”'s. Mini-invasive. Surg. 2020, 4, 57. http://dx.doi.org/10.20517/2574-1225.2020.44
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 14 clicks
Cite This Article 14 clicks














Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.