How to access the common bile duct
Abstract
Biliary access is a prerequisite to all endoscopic interventions in the biliary tract. Successful cannulation of the papilla of Vater is the predominant challenge for the majority of endoscopists training in endoscopic retrograde cholangiopancreaticography (ERCP), and the skills required for success differ substantially from those of regular luminal endoscopy. This paper reviews some of the key elements to successful biliary cannulation, a range of options for problem-solving when cannulation is difficult, and some tips and tricks in select special situations as well. The techniques are described, and available evidence is reviewed.
Keywords
INTRODUCTION
Endoscopic retrograde cholangiopancreaticography (ERCP) has since its inception 50 years ago been considered one of the most sophisticated, challenging and risky endoscopy procedures. Although recent advances in available accessories and imaging have reduced risks, it remains a complex procedure, requiring skills and training different from luminal endoscopy, from where most endoscopists arrive. It also requires access to - and understanding of - cross-sectional imaging and ductal anatomy.
The procedure may include a number of different elements, but common to all is the necessity to cannulate the papilla and achieve deep access to the desired duct, most often the bile duct. Successful cannulation of the native papilla is usually the primary obstacle of novice endoscopists, and even in expert hands, it may sometimes be hampered by unsuspected and even insurmountable problems. Failed cannulation is reported in up to 20% of cases[1], and increases the risk of most complications relevant to ERCP[2]. Although “no size fits all”, some of the techniques of selective biliary cannulation are universally useful and their special features and challenges, as well as the evidence to support them, are described in the following.
STANDARD CANNULATION
Papillary access and positioning
The passage of the duodenoscope into the second part of the duodenum and positioning it appropriately is usually not a challenge beyond the first training cases, but on occasion it can pose its own difficulties. Anatomical variants, such as cascade stomach or huge hiatal hernia, may complicate traversing the stomach, left-sided liver resections may hamper the passage of the pylorus and duodenal bulb, and gastric outlet obstruction or duodenal stenoses may also pose problems. Positional change, evacuation of air from the stomach, and on occasion guiding catheters or even large caliber balloon placement deep in the duodenum can facilitate the passage of the endoscope.
Papillary assessment
Visualizing the papilla is also mostly straightforward. However, duodenal obstruction, mucosal edema (e.g., in the setting of acute pancreatitis), aberrant position of the papilla or periampullary diverticulum may be a challenge. In most cases, minute observation of the duodenal wall, together with identification of the longitudinal mucosal fold leading up to the papilla, will succeed, even for papillae hidden under a fold or inside a diverticulum.
Once in position, care must be taken to observe the anatomy of the papilla, particularly as regards size, papillary orifice, and assumed direction of the bile duct. Once manipulated with the catheter, these may all change, and the native appearance is the most useful one. Photo-documentation is helpful for potential repeat procedures.
Guidewire cannulation
Cannulation can be done with a variety of catheters, and include a variety of guidewires[1]. Increasingly, however, a standard sphincterotome is used, for two reasons: the added utility of bending (+/- rotation) allows for a wider variety of targeting angles, and in the majority of ERCP procedures, a sphincterotomy will be performed as part of the therapeutic measures anyway. Thus, other special variants (e.g., super-tapered catheters, double-bending catheters, etc.) have a limited role today.
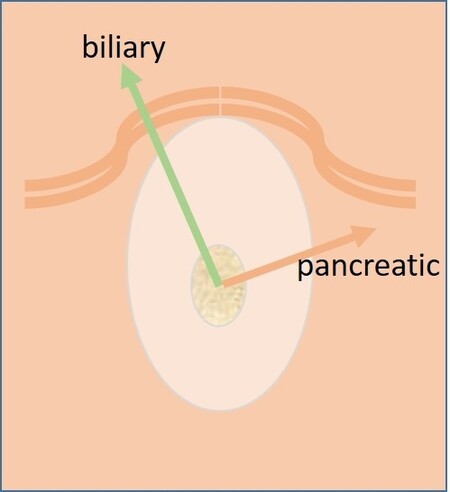
The bent sphincterotome tip can usually be rotated to the desired angle, which for the bile duct is normal around 11 o’clock [Figure 1]. However, care must be taken to relate this to the direction of the upward ductal impression if visible, or the orientation of the duodenal lumen.
For many years, wire-guided vs. contrast-guided cannulation have been compared and debated. Initially, contrast guidance was the only option, but with the increasing role of guidewires, their use also for cannulation has gained momentum. The concern with contrast has been the potentially harmful effect of inadvertent pancreatic contrast injection. Additionally, the guiding/stiffening role of the guidewire prior to catheter insertion may simplify the entry and increase the chance for successful access.
A number of comparative studies have been published, with all the inherent pitfalls in non-blindable technique comparisons[3]. Most reviews and meta-analyses conclude that guidewire-assisted cannulation is associated with a higher cannulation success rate, as well as a lower overall risk of post-ERCP pancreatitis (PEP)[4]. Consequently, the current European guidelines support this as the method of choice[2]. However, in difficult cases, delicate injection of a small amount of contrast may outline the detail of mural intraduodenal ductal anatomy, without significant pancreatic contrast filling. This can then guide the subsequent guidewire manipulation in the appropriate direction.
Two variants of the wire-assisted technique, the “touch technique” and the “non-touch technique” are described[4]. With the “touch technique”, the tip of the catheter is impacted gently into the papillary orifice in the appropriate direction, supporting the subsequent introduction of the guidewire. With the “non-touch technique”, the guidewire is positioned slightly protruding from the tip of the catheter and is inserted directly into the papilla and subsequently bile duct. This offers less support, but potentially avoids the mechanical distortion of the papillary anatomy that catheter impaction may cause[5]. One randomized controlled trial (RCT) comparing the two indicated a better cannulation success with the touch-technique, albeit with a higher risk of inadvertent pancreatic cannulations[6]. Most likely, both may have advantages depending on the papillary anatomy and experience of the endoscopist.
Once the guidewire passes, the direction will indicate what duct has been accessed, with the 11-12 o’clock direction towards the liver indicating biliary access. Care must be taken however, especially in the context of ampullary or pancreatic head tumors, where ductal anatomy may be distorted, or false routes can occur in the setting of necrotic tumors. Careful contrast injection will help confirm the situation.
As for the choice of guidewire for cannulation purposes, a number of options exist, in terms of caliber, material and shape[4]. For main papilla cannulation, the shape and tip stiffness are probably the primary concerns. It has been suggested that smaller is of benefit, but comparisons have failed to corroborate this[7], and the lesser axial support of thinner wires may be a disadvantage in subsequent maneuvers. Again, choice mostly comes down to personal preference and experience. A special variant for cannulation support, the “loop-tip” guidewire, was introduced to support passage through the crevices of the papilla[8], but it has since been discontinued.
DIFFICULT CANNULATION
The majority of cannulation attempts are straightforward in expert hands, even in native papillae. However, difficulties occur for both expected and unforeseen reasons. Difficult cannulations add to the risk of complications[9], and much effort has been channelled into this area since predicting difficult cannulations might allow pre-emptive measures to minimise adverse outcomes.
A variety of definitions have been suggested for what should be considered difficult. Since it is not always based on identifiable pre-procedural factors, recent definitions are instead based on features of the actual cannulation attempt. A study from Scandinavia looked at 907 ERCPs in native papillae in a multicenter study[10]. Allocating PEP as the determining factor, difficult cannulation was identified as > 5 min duration of attempt to cannulate, > 5 passes at the papilla, or > 2 guidewire passages into the pancreatic duct (PD). These three factors alone, or in combination, were associated with a significant increase in the incidence of PEP.
One important utility of such a definition is to aid the decision to change the initial strategy of standard guidewire cannulation. Further persistence with the same technique may finally succeed, but it is likely to increase the complication risk, so changing the strategy earlier should be considered.
There are number of alternative methods to achieve cannulation success that may be used instead of, or along with, the initial approach. Common to these techniques are that they require additional skills, add risk, but increase the chance of eventual cannulation success.
Double-wire technique
Not infrequently, attempts to access the bile duct result in inadvertent guidewire placement in the PD. If this recurs or results after substantial struggle, leaving it there and proceeding with cannulation alongside with another wire preloaded in the catheter, the “double wire technique” (DWT) is a viable option. In theory, the pancreatic wire stabilizes a mobile papilla, straightens the intraduodenal segment of the ducts, and potentially causes partial blockage of the PD, all components that may increase the chance of subsequent access to the bile duct. The method was introduced more than 20 years ago[11] and has repeatedly been shown to improve cannulation success. The technique has been modified to include placement of a small-calibre transpapillary pancreatic stent over the guidewire already in the PD, resulting in significant protection from PEP[12], and is currently recommended in recent ESGE guideline on ERCP adverse events[13] whenever the DWT is used. Alternatively, a stent can be placed initially in the PD for subsequent alongside-cannulation or needle knife cutting on the stent.
DWT has been associated with increased risk of PEP. In a recent systematic review comprising 7 RCTs with difficult cannulation in 577 patients, the authors found a 2-fold increase in risk of PEP using the DWT, without increased cannulation success[14]. However, like all problem-solving methods, it may falsely be blamed for the risk imposed by previous failed cannulation attempts. Also, most studies in that review were done prior to the standard use of rectal non-steroidal, anti-inflammatory drugs (NSAIDs) for PEP prophylaxis. The protective role of a pancreatic stent in combination with NSAIDs is not clear[13].
Transpancreatic sphincterotomy
Another potential utility of a pancreatic access wire is to perform a wire-guided pancreatic sphincterotomy, effectively also cutting the common ampullary muscle. The technique allows for a more focused cut than the free-hand needle knife precut technique, probably reducing the risk of perforation, and frequently, the biliary orifice can be visualized on the left edge of the cut crevice. Alternatively, an additional transverse free-hand extension of the cut to the left can be performed. The method was spearheaded by the Helsinki group, who showed that the method compared favorably to free-hand precut in a large retrospective multi-center trial[15]. More recently, a systematic review also concluded that the method offered a higher cannulation success rate compared to the relevant alternatives, with a similar complication rate[16]. A recent randomized comparison found a comparable PEP risk, but a higher cannulation success rate (85% vs. 70%) in transpancreatic sphincterotomy vs. double-wire technique[17]. Long-term follow-up data are lacking at this time.
Needle knife precut
Classic precut technique
Without PD wire access, utilizing a needle knife to gain access to the bile duct must be considered. In this technique, the roof of the papilla is dissected layer by layer from the top of the mound, in the assumed direction of the bile duct [Figure 1], until the whitish onion-skin appearance of the bile duct epithelium is evident. The orifice can then usually be identified as a tiny nipple downstream, for subsequent cutting or cannulation, usually with a guidewire[18]. The method requires visual exposure of the tissues, so sufficiently deep dissection is necessary, while avoiding transmural cut with duodenal perforation. The feasibility and safety of the method depends on the size of the intraduodenal papillary portion, with small, flat or hidden papillae leaving less space for cutting[2].
Data on precut success and safety vary widely, surely depending on technique and expertise, but also on timing, sooner being safer. Initial statements on increased PEP risk have been somewhat countered by more recent meta-analyses, particularly considering early precut vs. persistent cannulation attempts[19]. Most studies and guidelines state the need for expertise to safely perform biliary precut, but the training phase obviously poses a concern. Precut does remain a potentially risky method and should not replace good cannulation technique.
Needle knife fistulotomy
Suprapapillary fistulotomy is incision of the bile duct above the papillary orifice, onto the duodenal protrusion of the bile duct, creating a direct fistular access to the bile duct independently of the papilla. Subsequent maneuvers can then be performed through this orifice, or prograde extension of the fistula across the papillary muscle can be made.
The method has the potential benefit of biliary access without touching the pancreatic orifice, thus reducing the risk of PEP. Indeed, in the meta-analysis by Choudhary et al.[19], a distinct reduction in PEP was seen with this method. However, its feasibility depends on anatomical factors and ideally a dilated bile duct down toward the papilla, to increase the chance of successful bile duct puncture. Ampullary cancer represents a special situation where the method can indeed be useful[20].
SPECIAL PROBLEMS
Periampullary diverticula
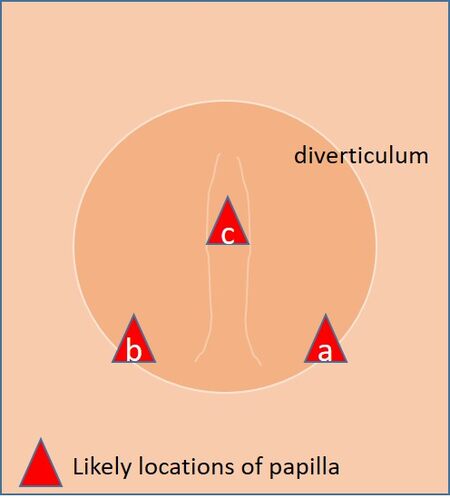
Duodenal diverticula are relatively common, particularly in elderly patients[21]. Moreover, both advancing age and the presence of the diverticulum promote the preferential growth of glucuronidase-producing bacteria predisposing to the formation of gallstones[22]. Periampullary diverticula with an extradiverticular position of the papilla rarely cause concern, although the trajectory of the ducts may change. Intradiverticular papillae can be more difficult to locate and approach, particularly those located on the inner edge of the lower rim. Mostly, intradiverticular papillae can be found at the lower edge, 5 o’clock or 7 o’clock, or on central intradiverticular fold, if there is one [Figure 2]. Entry of the diverticulum with the tip of the scope is helpful if feasible, otherwise, clipping, mini-biopsy forceps alongside the cannulating catheter or saline injection to lift the papilla forward may all help in facilitating the cannulation. Inadvertent wire passage into the pancreatic duct should always be retained for added support and subsequent biliary access. In general, published results indicate a similar success rate in these patients[23], although time spent may be longer.
Billroth II anatomy
Billroth II resections were prevalent as definitive peptic ulcer therapy in the pre-PPI era, but we still see these patients occasionally presenting for ERCP. Access is usually feasible with a standard duodenoscope, although fixations in the afferent loop may pose a risk for perforation during intubation and justify the change to an enteroscope. A standard gastroscope or pediatric colonoscope with a cap are valid options, but manipulation at the level of the papilla are more cumbersome. With a side-viewing instrument, positioning at the papilla is usually straightforward, although the access from below renders everything upside down. This also makes the standard sphincterotome less useful because the direction of the bending and the cutting wire end up on the wrong side. Usually, a straight standard catheter with a guidewire is preferrable for cannulation. For sphincterotomy, special inverted sphinterotomes are available, but needle knife cutting over a temporary short plastic stent may be a more available and simpler alternative[24].
Other anatomy - intact papilla
Gastric resection (for cancer) and diversion (bariatric gastric bypass) both comprise a Roux-en-Y loop connected to the distal esophagus, with a reconnected jejunal loop of variable length leading to the duodenum from below, similar to the Billroth II anatomy. This situation presents access challenges, as well as issues at the level of the papilla.
In these cases, device-assisted enteroscopes are usually necessary[25]. Access to the entero-enteric anastomosis is usually straightforward, avoiding the passage of the stomach and ligament of Treitz. With visual control of the anastomosis, the correct loop would be the one connected to the blind loop, usually at an acute angle to the scope direction. Further passage will be variably complex depending on the length of the loop and the Treitz angulation, or other fixations may be additional challenges. Also, the amount of small bowel loops makes tip manipulation limited. Typically, the access to the papilla requires a 180 degrees angulation at the level of the lower duodenal knee. A cap on the scope tip facilitates manipulation of the papilla and is mostly helpful. Regardless, cannulation (usually with a straight catheter) is a challenge, also given the lack of an instrument channel elevator on the enteroscope.
Published data confirm the technical challenges of access, as well as cannulation[26]. Thus, percutaneous, hybrid laparoscopic approaches, as well as endoscopic ultrasound (EUS)-assisted approaches, are being explored, depending on the specific surgical situation[27]. As these procedures become increasingly common and as weight loss predisposes to the formation of gallstones, data and technical developments in this important field are eagerly awaited.
Other anatomy - hepaticojejunostomy
The other relevant anatomical situation is a Roux-en-Y hepaticojejunostomy, either with an entero-enterostomy, e.g., after hepatobiliary surgery complications or liver transplantations, or after Whipple surgery. In both situations, enteroscopes are usually needed for enteric passage. However, biliary access via a hepaticojejunostomy is usually less demanding, although identification, as well as cannulation of strictured anastomoses may be a challenge. Again, EUS-guided alternatives are being explored, particularly for palliative situations.
Other options
After prolonged failed attempts at biliary cannulation, the endoscopists must always consider alternatives: call a friend or stop and try another day. Depending on the urgency of the clinical situation, the reasons for failure and the access to more experienced colleagues are both options that must be considered. The overall benefit of the patient must be paramount. If drainage is urgently needed, EUS-guided, as well as percutaneous techniques must also be considered, depending on available expertise.
Conclusions
Most biliary cannulations are straightforward given the appropriate expertise. However, difficulties occur because of specific anatomical difficulties or even because of specifics of the papillary anatomy. Comprehensive understanding of the situation, and appropriate command of the various problem-solving options are mandatory and must be part of the procedural armamentarium of all endoscopists performing ERCP.
DECLARATIONS
Authors’ contributionsDeveloped the concept, researched the field, and prepared the manuscript: Aabakken L
Developed the concept, researched the field, and edited and supplemented the manuscript: Bhat P
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestBoth authors have no conflict of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2021.
REFERENCES
1. Freeman ML, Guda NM. ERCP cannulation: a review of reported techniques. Gastrointest Endosc 2005;61:112-25.
2. Testoni PA, Mariani A, Aabakken L, et al. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2016;48:657-83.
3. Tse F, Yuan Y, Moayyedi P, Leontiadis GI. Guide wire-assisted cannulation for the prevention of post-ERCP pancreatitis: a systematic review and meta-analysis. Endoscopy 2013;45:605-18.
4. Cennamo V, Bassi M, Landi S, et al. Wire-guided biliary cannulation: a comprehensive approach to a set of techniques. Eur J Gastroenterol Hepatol 2019;31:1299-305.
5. Nambu T, Ukita T, Shigoka H, Omuta S, Maetani I. Wire-guided selective cannulation of the bile duct with a sphincterotome: a prospective randomized comparative study with the standard method. Scand J Gastroenterol 2011;46:109-15.
6. Bassi M, Luigiano C, Ghersi S, et al. A multicenter randomized trial comparing the use of touch versus no-touch guidewire technique for deep biliary cannulation: the TNT study. Gastrointest Endosc 2018;87:196-201.
7. Albert JG, Lucas K, Filmann N, et al. A novel, stiff-shaft, flexible-tip guidewire for cannulation of biliary stricture during endoscopic retrograde cholangiopancreatography: a randomized trial. Endoscopy 2014;46:857-61.
8. Masci E, Mangiavillano B, Luigiano C, et al. Comparison between loop-tip guidewire-assisted and conventional endoscopic cannulation in high risk patients. Endosc Int Open 2015;3:E464-70.
9. Berry R, Han JY, Tabibian JH. Difficult biliary cannulation: Historical perspective, practical updates, and guide for the endoscopist. World J Gastrointest Endosc 2019;11:5-21.
10. Halttunen J, Meisner S, Aabakken L, et al. Difficult cannulation as defined by a prospective study of the Scandinavian Association for Digestive Endoscopy (SADE) in 907 ERCPs. Scand J Gastroenterol 2014;49:752-8.
11. Dumonceau JM, Devière J, Cremer M. A new method of achieving deep cannulation of the common bile duct during endoscopic retrograde cholangiopancreatography. Endoscopy 1998;30:S80.
12. Phillip V, Pukitis A, Epstein A, et al. Pancreatic stenting to prevent post-ERCP pancreatitis: a randomized multicenter trial. Endosc Int Open 2019;7:E860-8.
13. Dumonceau JM, Kapral C, Aabakken L, et al. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2020;52:127-49.
14. Tse F, Yuan Y, Moayyedi P, Leontiadis GI, Barkun AN. Double-guidewire technique in difficult biliary cannulation for the prevention of post-ERCP pancreatitis: a systematic review and meta-analysis. Endoscopy 2017;49:15-26.
15. Halttunen J, Keränen I, Udd M, Kylänpää L. Pancreatic sphincterotomy versus needle knife precut in difficult biliary cannulation. Surg Endosc 2009;23:745-9.
16. Pécsi D, Farkas N, Hegyi P, et al. Transpancreatic Sphincterotomy Is Effective and Safe in Expert Hands on the Short Term. Dig Dis Sci 2019;64:2429-44.
17. Kylänpää L, Koskensalo V, Saarela A, et al. Transpancreatic biliary sphincterotomy versus double guidewire in difficult biliary cannulation: a randomized controlled trial. Endoscopy 2021; doi: 10.1055/a-1327-2025.
18. Davee T, Garcia JA, Baron TH. Precut sphincterotomy for selective biliary duct cannulation during endoscopic retrograde cholangiopancreatography. Annals of gastroenterology. 2012;25(4):291-302.
19. Choudhary A, Winn J, Siddique S, et al. Effect of precut sphincterotomy on post-endoscopic retrograde cholangiopancreatography pancreatitis: a systematic review and meta-analysis. World J Gastroenterol 2014;20:4093-101.
20. Aabakken L, Osnes M. Endoscopic choledochoduodenostomy (ECDT) as palliative treatment of malignant periampullary obstructions of the common bile duct: a follow-up study. Gastrointest Endosc 1986;32:41-2.
21. Tyagi P, Sharma P, Sharma BC, Puri AS. Periampullary diverticula and technical success of endoscopic retrograde cholangiopancreatography. Surg Endosc 2009;23:1342-5.
22. Skar V, Skar AG, Bratlie J, Osnes M. Beta-glucuronidase activity in the bile of gallstone patients both with and without duodenal diverticula. Scand J Gastroenterol 1989;24:205-12.
23. Boix J, Lorenzo-Zúñiga V, Añaños F, Domènech E, Morillas RM, Gassull MA. Impact of periampullary duodenal diverticula at endoscopic retrograde cholangiopancreatography: a proposed classification of periampullary duodenal diverticula. Surg Laparosc Endosc Percutan Tech 2006;16:208-11.
24. Osnes M, Rosseland AR, Aabakken L. Endoscopic retrograde cholangiography and endoscopic papillotomy in patients with a previous Billroth-II resection. Gut 1986;27:1193-8.
25. Aabakken L, Bretthauer M, Line PD. Double-balloon enteroscopy for endoscopic retrograde cholangiography in patients with a Roux-en-Y anastomosis. Endoscopy 2007;39:1068-71.
26. Tanisaka Y, Ryozawa S, Mizuide M, et al. Status of single-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: Systematic review and meta-analysis on biliary interventions. Dig Endosc 2020; doi: 10.1111/den.13878.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Aabakken L, Bhat P. How to access the common bile duct. Mini-invasive Surg 2021;5:25. http://dx.doi.org/10.20517/2574-1225.2021.09
AMA Style
Aabakken L, Bhat P. How to access the common bile duct. Mini-invasive Surgery. 2021; 5: 25. http://dx.doi.org/10.20517/2574-1225.2021.09
Chicago/Turabian Style
Aabakken, Lars, Purnima Bhat. 2021. "How to access the common bile duct" Mini-invasive Surgery. 5: 25. http://dx.doi.org/10.20517/2574-1225.2021.09
ACS Style
Aabakken, L.; Bhat P. How to access the common bile duct. Mini-invasive. Surg. 2021, 5, 25. http://dx.doi.org/10.20517/2574-1225.2021.09
About This Article
Special Issue
Copyright
Data & Comments
Data

 Cite This Article 20 clicks
Cite This Article 20 clicks










Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.