Oligometastatic prostate cancer: a new horizon for robotic radical prostatectomy
Abstract
The advent of modern diagnostic techniques and improved patient monitoring in the setting of clinical trials has led to an increased diagnosis of oligometastatic prostate cancer (OMPC), defined as three-to-five metastatic deposits in a single organ or multiple organs. OMPC is increasingly diagnosed in men who were in the past considered to have organ-confined disease. OMPC occurs at the transition between localized prostate cancer and widespread metastases. Our review evaluates the available evidence regarding robot-assisted cytoreductive prostatectomy feasibility and oncological outcomes in oligometastatic settings. We also consider the limitations and future directions for this approach. We performed a non-systematic PubMed and Google Scholar search. We screened pertinent studies published from 2014 up to May 2021. Our search identified 524 records. After excluding duplication, 54 full-text articles were identified and were screened for eligibility. We found nine papers (863 patients) that met the inclusion criteria for the review. The outcomes evaluated were 1-, 3-, and 5-year progression-free survival, cancer-specific and overall survival rates. Our review article demonstrates the feasibility and safety of Robot-assisted radical prostatectomy in patients with OMPC with proven oncological benefits. Prospective studies are ongoing and may provide further solid evidence.
Keywords
INTRODUCTION
Oligometastatic prostate cancer (OMPC) is generally defined as cancer in patients with 3-5 metastatic deposits in a single organ or multiple organs on conventional imaging. With the advent of modern diagnostic techniques and improved patient monitoring in the setting of clinical trials, OMPC is increasingly diagnosed in men who were in the past considered to have organ-confined disease[1,2]. OMPC occurs at the transition between localized prostate cancer and widespread metastases. Recent data suggest that molecular differences exist between OMPC and polymetastatic prostate cancer (PMPC) {metastases at > 5 sites}. It is known, as well, that OMPC patient populations behave differently from PMPC in the clinical setting[3-5]. A compelling difference in overall survival in men with OMPC vs. PMPC has also been shown (< 5 metastases at the time of diagnosis)[6].
Men with localized prostate cancer are managed with active surveillance, focal therapy, or radical therapy, either radical prostatectomy or radiotherapy[7]. Robot-assisted radical prostatectomy (RARP) is the most common form of surgical treatment for localized prostate cancer. The current standard of care for men with metastatic prostate cancer (MPC) is chemohormonal therapy or androgen deprivation therapy with/without abiraterone acetate/prednisone[8]. Treatment of a primary tumor in the metastatic setting is pursued only as a palliative measure (e.g., patients with significant local symptoms secondary to primary tumor)[9]. It is biologically feasible, however, that an unchecked local tumor may encourage the progression of metastases, possibly acting as a source for tumor seeding, which has been shown in other types of metastatic cancer. This would mean that the longer the primary tumor remains in the body, the greater the chances of new metastatic deposits[10]. It is logical to say that treating primary tumor can delay the progression of metastases and improve survival in men with MPC.
Regardless of unsatisfactory evidence from survival statistics, local treatment is sometimes used in the management of OMPC. Our review evaluates the available evidence regarding robot-assisted cytoreductive prostatectomy (CRP) feasibility and oncological outcomes in oligometastatic settings. We also consider the limitations and future directions for this approach.
EVIDENCE ACQUISITION AND SEARCH STRATEGY
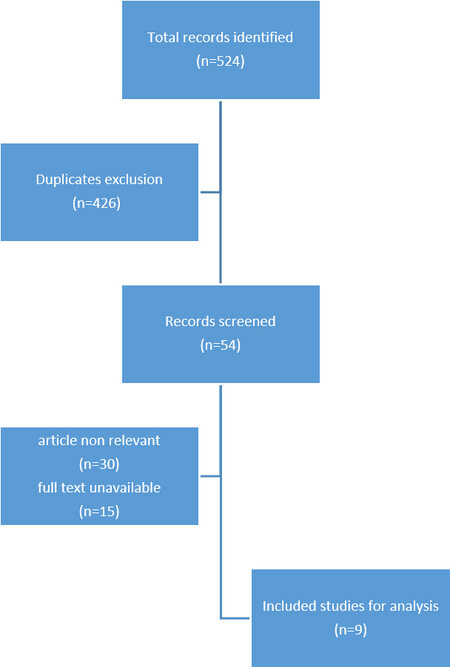
A non-systematic PubMed and Google Scholar search were performed for English language publications from January 2014 to May 2021. Key search terms included “prostate cancer” and “oligometastatic” or “cytoreductive prostatectomy” or “robot-assisted prostatectomy” AND “oligometastatic”. At first, we searched the abstracts of studies for relevant inclusion. Next, we retrieved full-text original articles from the selected abstracts. We utilized two reviewers (VW, FB) to independently assess abstracts and original articles for eligibility. We classified the relevant materials as inclusion, unsure, or exclusion. In the case of dispute between the two reviewers, consensus was reached to resolve the difference of opinion. Detailed screening of relevant full-text-articles’ references was performed to identify additional pertinent articles not found in the PubMed database and through Google Scholar. Following studies were excluded: non-relevant or partially relevant secondary publications and systematic reviews, unavailable full-text articles. Figure 1 demonstrates flow chart of search strategy and final number of articles included in the current review.
Studies were eligible for inclusion in our review if they included patients who opted for open or robot-assisted cytoreductive prostatectomy for histologically proven prostate cancer and evidence of oligometastatic disease on relevant imaging or biopsy. As a primary outcome, we evaluated whether the proposed open or robot-assisted CRP was associated with progression-free survival (PFS), cancer-specific survival (CSS) or overall survival (OS). Studies without CRP or oncological outcomes were excluded.
Definition of progression
PFS was defined as the time from starting androgen deprivation therapy to the evidence of biochemical or clinical progression. Biochemical progression was defined as two consecutive PSA readings ≥ 0.2 ng/mL separated by 2-week intervals if PSA decreased to undetectable serum levels postoperatively. Clinical progression was determined as the onset of new symptoms due to local progression or distant metastases. CSS was defined as the time from prostate cancer diagnosis to death related to prostate cancer events. OS was defined as the time from prostate cancer diagnosis to death from any noncancer-related cause.
DATA-EXTRACTION
Table 1 shows the summary of included studies that were finalized after evidence acquisition and search strategy. It involves sample size, study design, the definition of OMPC, and the selected approach - CRP, PFS, CCS, and OS [Table 1].
Summary of studies using CRP for OMPC
| Authors | Study type | OMPC criteria (DM) | n | PFS | CSS | OS | Functional outcome | SRC (details) |
| Heidenreich et al.[7] (2018) | Retrospective | ≤ 3 Bone (CT, SS) | 104 (O-CRP) 9 (RA-CRP) | NR | 89% at 3 years; 81% at 5 years | 80% at 5 years | 68% UC at 12 months | 9% (5% - RL for bleeding; 4%-LD) |
| Sooriakumaran et al.[11] (2016) | Retrospective | M1a-M1b (CT, SS) | 106 (O-CRP) | NR | NR | 89% at 23 months | 64% UC at 3 months | 19% (14%-BT; 5%-LD) |
| Jang et al.[12] (2018) | Retrospective | ≤ 5 Bone (SS) | 38 (RA-CRP) 41 (NLT) | 75% (RA-CRP) vs. 40% (NLT) at 40 months | NR | NR | NR | 13% (8%-BT; 5%-RL for rectal injury; bleeding) |
| Culp et al.[13] (2014) | Population based | M1a-M1c (NR) | 245 (O-CRP) 7811 (nCRP) | NR | 76% (RP) vs. 61% (nCRP) at 5 years | 67% (RP) vs. 53% (nCRP) at 5 years | NR | NR |
| Antwi and Everson[17] (2014) | Population based | M1a-M1c (SS) | 222 (O-CRP) | NR | 85% | 82% | NR | NR |
| Gratzke et al.[16] (2014) | Population based | M1 (SS) | 74 (O-CRP) 7811 (NLT) | NR | NR | 55% (RP) vs. 21% (NLT) at 5 years | NR | NR |
| Satkunasivam et al.[15] (2015) | Population based | M1 (CT, SS) | 47 (O-CRP) | NR | 79% at 3 years | 73% at 3 years | NR | NR |
| Gandaglia et al.[14] (2016) | Retrospective | ≤ 5 Bone (CT/MRI, SS) | 11 (RA-CRP) | NR | 82% at 7 years | NR | NR | 82% (73%-BT, 9%-RL for anastomotic leakage) |
| Poelaert et al.[18] (2017) | Prospective | < 4 Bone (SS) | 1 (O-CRP) 15 (RA-CRP) 9 (NLT) | NR | 100% (RP) vs. 61% (NLT) at 2 years | 100% (RP) vs. 51% (NLT) at 2 years | 49% UC at 3 months | 0% |
RESULTS
Our search identified 524 records. After excluding duplication, 54 full-text articles were identified and were screened for eligibility. We found nine papers (863 patients) that met the inclusion criteria for the review. Four studies were retrospective; four were population-based. One study was prospective.
Heidenreich et al.[7] assessed 113 patients with osseous MPC who underwent CRP. The results showed 80% 5-year OS, 9% risk of surgery-related complications, and 68% urinary continence at 12 months after CRP. Sooriakumaran et al.[11] retrospectively assessed 106 patients with MPC who underwent CRP with extended lymphadenectomy. They reported 89% OS at 23 months, 64% urinary continence at 3 months, and 14% surgery-related complications. Jang et al.[12] retrospectively reviewed records of 79 men with OMPC, 38 of whom underwent robot-assisted CRP. They found 75% PFS in patients with RA-CRP vs. 40% PFS in men without RA-CRP at 40 months. Additionally, 5% of men experienced surgery-related complications in the RA-CRP group. Culp et al.[13] used a population-based SEER database of 8185 men with MPC of whom 245 underwent CRP. They reported CSS of 76% in CRP vs. 61% with non-CRP men at 5 years. The authors also noted OS at 5 years at 67% in the CRP group vs. 53% in the non-CRP group. Gandaglia et al.[14] analyzed perioperative and long-term (7 years) oncologic outcomes of radical prostatectomy in a selected cohort of 11 patients with OMPC treated with RP and extended pelvic lymph node dissection. PFS was 45% and CSM was 82% with 18% of grade 3 post-operative complications. Satkunasivam et al.[15] assessed survival following local therapy in comparison with no local therapy for 4069 men with metastatic prostate cancer from the SEER-Medicare linked database. RP compared to NLT was associated with a 52% reduction in the risk of prostate cancer-specific mortality (HR = 0.48, 95%CI: 0.27-0.85). OS at 3 years was 73% for RP.
DISCUSSION
Robot-assisted radical prostatectomy (RARP) is the most common form of treatment in men with organ-confined prostate cancer[19]. RARP has shown promising results in locally advanced prostate cancer treatment[20]. Here we reviewed 9 papers (4 retrospective, 4 population-based and 1 prospective) for oncological and functional outcomes of cytoreductive radical prostatectomy (open or robot-assisted) in OMPC settings. We identified 3 key themes: (1) improved overall survival statistics (PFS, OS, CSS) are seen after CRP for men with OMPC compared to men without CRP; (2) CPR is shown to be feasible and safe (fewer surgery-related complication rates with acceptable functional outcomes) with cytoreductive prostatectomy in OMPC settings; and (3) an emerging role for robot-assisted cytoreductive prostatectomy in selected men with OMPC.
Men diagnosed with metastatic prostate cancer usually receive systemic therapy, such as androgen deprivation therapy and chemotherapy, while radical prostatectomy is typically reserved for localized prostate cancers. However, Tzelepi et al.[21] demonstrated the intra-prostatic survival of lethal prostate cancer cell clones with the biological potential to metastasize despite systemic therapy. A growing body of evidence suggests that control of a primary tumor may delay the progress of metastases, thereby improving overall survival and reducing prostate cancer-specific mortality. Recently systematic review and meta-analysis were conducted that compared CRP to systemic and radiation therapy in the treatment of OMPC. This systematic review showed that CRP had significantly higher 1-, 3-, and 5-year CSS and OS rates compared to systemic therapy[22]. This review of the current literature also demonstrated that men with OMPC experience improved PFS, OS, and CSS after CRP.
Preisser et al.[23] compared perioperative results between CRP and RP for localized prostate cancer and reported that CRP results in more complications and longer hospital stays. However, CRP also reduces long-term local complications, including bleeding, bladder outlet obstruction, and ureteral obstruction. Published results of CR-related complication rates were 20% compared to 53% for systemic therapy and 47% for men who received radiotherapy. Surgery complication rates in our review series ranged from 5%-18%.
The debate surrounding RARP vs. ORP is unlikely to have a clear resolution soon, but an increasing number of surgeons are trained in, and routinely perform, RARP. The benefits of the technique have been described for nerve sparing and continence or sexual function preservation, and the robotic approach continues to gain acceptance for a larger number of indications. Numerous studies show that the robotic approach is increasingly becoming the first-choice strategy of urologists, even in metastatic cases[24]. In a 2010 study on CRP for OMPC patients, only 9 robotic CRP procedures were conducted vs. 104 open procedures[7]. Just a few years later, Sooriakumaran et al.[11] conducted a multicenter study where the choice of approach was left to the clinician’s discretion and in one center, all 5 procedures (100%) were performed with robot-assisted procedures. In 2017 as described in Jang et al.[12], 38 robotic surgeries were assessed; followed by Poelaert et al.[18] who described the outcomes of 17 patients, 16 of whom underwent robotically assisted CPR. In this study, the authors found return of 70.6% continence with no local symptoms in the surgery group vs. 44.8% in the non-RARP group (P = 0.014). Obstructive voiding with the need for medical intervention was present in 37.9% of patients who did not have robotic surgery and 6.8% had ureteric obstruction with 3.4% requiring JJ-stenting. Three months after CRP, 29.4% and 11.8% of patients suffered grade 1 and 2 complications, respectively. Robotic surgery was shown to be as safe in OMPC as in non-metastatic disease with acceptable surgical morbidity and oncological outcomes. In Poelaert et al.[18], there were no high-grade (> grade 2) complications. While 41.2% of patients suffered low-grade complications, outcomes appeared to be improved over the Heidenreich et al.[7] open CRP series with a lower 39.1% complication rate, but with 13% of patients experiencing grade 3 complications. A recent randomized controlled trial of surgery plus best systemic therapy vs. best systematic therapy alone for men with OMPC has completed accrual in the UK (the TROMBONE trial) and is currently awaiting publication[25].
CONCLUSION
Reviewing the relevant literature, we find that RP and RARP in particular, appear to be feasible and safe for patients diagnosed with oligometastatic prostate cancer, providing oncological benefit for this growing population of patients with low volume metastasis. Future studies should address the selection of patients for potential multimodal therapeutic strategies.
DECLARATIONS
AcknowledgmentWe thank Ms. Sima Rabinowitz for editorial assistance.
Authors’ contributionsMade substantial contributions to conception and design of the study and manuscript writing: Wagaskar VG, Barthe F
Manuscript reviewing and critical analysis: Sooriakumaran P, Martini A
Contributed to manuscript writing as well as provided administrative, technical, and material support: Tewari A
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestDr. Tewari A has served as a site-PI on pharma/industry-sponsored clinical trials from Kite Pharma, Lumicell Inc, Dendreon, and Oncovir Inc. He has received research funding (grants) to his institution from DOD, NIH, Axogen, Intuitive Surgical, AMBFF, and other philanthropy. Dr. Tewari A has served as an unpaid consultant to Roivant Biosciences and advisor to Promaxo. He owns equity in Promaxo. Other authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2022.
REFERENCES
2. Evangelista L, Briganti A, Fanti S, et al. New clinical indications for (18)F/(11)C-choline, new tracers for positron emission tomography and a promising hybrid device for prostate cancer staging: a systematic review of the literature. Eur Urol 2016;70:161-75.
3. Ost P, Reynders D, Decaestecker K, et al. Surveillance or metastasis-directed therapy for oligometastatic prostate cancer recurrence: a prospective, randomized, multicenter phase II trial. J Clin Oncol 2018;36:446-53.
4. Gravis G, Boher JM, Chen YH, et al. Burden of metastatic castrate naive prostate cancer patients, to identify men more likely to benefit from early docetaxel: further analyses of CHAARTED and GETUG-AFU15 studies. Eur Urol 2018;73:847-55.
5. Parker CC, James ND, Brawley CD, et al. Radiotherapy to the primary tumour for newly diagnosed, metastatic prostate cancer (STAMPEDE): a randomised controlled phase 3 trial. Lancet 2018;392:2353-66.
6. Singh D, Yi WS, Brasacchio RA, et al. Is there a favorable subset of patients with prostate cancer who develop oligometastases? Int J Radiat Oncol Biol Phys 2004;58:3-10.
7. Heidenreich A, Fossati N, Pfister D, et al. Cytoreductive radical prostatectomy in men with prostate cancer and skeletal metastases. Eur Urol Oncol 2018;1:46-53.
8. Cornford P, Bellmunt J, Bolla M, et al. EAU-ESTRO-SIOG guidelines on prostate cancer. Part II: treatment of relapsing, metastatic, and castration-resistant prostate cancer. Eur Urol 2017;71:630-42.
9. Mathieu R, Korn SM, Bensalah K, Kramer G, Shariat SF. Cytoreductive radical prostatectomy in metastatic prostate cancer: does it really make sense? World J Urol 2017;35:567-77.
10. Morrow M, Goldstein L. Surgery of the primary tumor in metastatic breast cancer: closing the barn door after the horse has bolted? J Clin Oncol 2006;24:2694-6.
11. Sooriakumaran P, Karnes J, Stief C, et al. A Multi-institutional analysis of perioperative outcomes in 106 men who underwent radical prostatectomy for distant metastatic prostate cancer at presentation. Eur Urol 2016;69:788-94.
12. Jang WS, Kim MS, Jeong WS, et al. Does robot-assisted radical prostatectomy benefit patients with prostate cancer and bone oligometastases? BJU Int 2018;121:225-31.
13. Culp SH, Schellhammer PF, Williams MB. Might men diagnosed with metastatic prostate cancer benefit from definitive treatment of the primary tumor? Eur Urol 2014;65:1058-66.
14. Gandaglia G, Fossati N, Stabile A, et al. Radical prostatectomy in men with oligometastatic prostate cancer: results of a single-institution series with long-term follow-up. Eur Urol 2017;72:289-92.
15. Satkunasivam R, Kim AE, Desai M, et al. Radical prostatectomy or external beam radiation therapy vs no local therapy for survival benefit in metastatic prostate cancer: a SEER-Medicare analysis. J Urol 2015;194:378-85.
16. Gratzke C, Engel J, Stief CG. Role of radical prostatectomy in metastatic prostate cancer: data from the Munich Cancer Registry. Eur Urol 2014;66:602-3.
17. Antwi S, Everson TM. Prognostic impact of definitive local therapy of the primary tumor in men with metastatic prostate cancer at diagnosis: a population-based, propensity score analysis. Cancer Epidemiol 2014;38:435-41.
18. Poelaert F, Verbaeys C, Rappe B, et al. Cytoreductive prostatectomy for metastatic prostate cancer: first lessons learned from the multicentric prospective local treatment of metastatic prostate cancer (LoMP) trial. Urology 2017;106:146-52.
19. Wagaskar VG, Mittal A, Sobotka S, et al. Hood technique for robotic radical prostatectomy-preserving periurethral anatomical structures in the space of Retzius and Sparing the pouch of Douglas, enabling early return of continence without compromising surgical margin rates. Eur Urol 2021;80:213-21.
20. Saika T, Miura N, Fukumoto T, Yanagihara Y, Miyauchi Y, Kikugawa T. Role of robot-assisted radical prostatectomy in locally advanced prostate cancer. Int J Urol 2018;25:30-5.
21. Tzelepi V, Efstathiou E, Wen S, et al. Persistent, biologically meaningful prostate cancer after 1 year of androgen ablation and docetaxel treatment. J Clin Oncol 2011;29:2574-81.
22. Shemshaki H, Al-Mamari SA, Geelani IA, Kumar S. Cytoreductive radical prostatectomy versus systemic therapy and radiation therapy in metastatic prostate cancer: a systematic review and meta-analysis. Urologia 2022;89:16-30.
23. Preisser F, Mazzone E, Nazzani S, et al. Comparison of perioperative outcomes between cytoreductive radical prostatectomy and radical prostatectomy for nonmetastatic prostate cancer. Eur Urol 2018;74:693-6.
24. Checcucci E, Amparore D, De Luca S, Autorino R, Fiori C, Porpiglia F. Precision prostate cancer surgery: an overview of new technologies and techniques. Minerva Urol Nefrol 2019;71:487-501.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Wagaskar VG, Barthe F, Martini A, Sooriakumaran P, Tewari A. Oligometastatic prostate cancer: a new horizon for robotic radical prostatectomy. Mini-invasive Surg 2022;6:14. http://dx.doi.org/10.20517/2574-1225.2021.106
AMA Style
Wagaskar VG, Barthe F, Martini A, Sooriakumaran P, Tewari A. Oligometastatic prostate cancer: a new horizon for robotic radical prostatectomy. Mini-invasive Surgery. 2022; 6: 14. http://dx.doi.org/10.20517/2574-1225.2021.106
Chicago/Turabian Style
Wagaskar, Vinayak G., Flora Barthe, Alberto Martini, Prasanna Sooriakumaran, Ash Tewari. 2022. "Oligometastatic prostate cancer: a new horizon for robotic radical prostatectomy" Mini-invasive Surgery. 6: 14. http://dx.doi.org/10.20517/2574-1225.2021.106
ACS Style
Wagaskar, VG.; Barthe F.; Martini A.; Sooriakumaran P.; Tewari A. Oligometastatic prostate cancer: a new horizon for robotic radical prostatectomy. Mini-invasive. Surg. 2022, 6, 14. http://dx.doi.org/10.20517/2574-1225.2021.106
About This Article
Special Issue
Copyright
Data & Comments
Data

 Cite This Article 12 clicks
Cite This Article 12 clicks










Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.