Cold snare polypectomy and underwater endoscopic mucosal resection for superficial nonampullary duodenal epithelial tumors
Abstract
Although the diagnostic and therapeutic opportunities for superficial nonampullary duodenal epithelial tumors (SNADETs) have been increasing, the natural history and treatment outcomes remain unclear. Due to the anatomical characteristics of the duodenum, clinicians should be more sensitive to the occurrence of complications for tumors in the duodenum compared to other gastrointestinal tumors. Recently, with the expectation of minimally invasive treatment, cold snare polypectomy (CSP) and underwater endoscopic mucosal resection (UEMR) have been accepted as simple and safe endoscopic treatments for SNADETs. In our institution, CSP achieved good treatment outcomes: a median procedure time of 3 (range, 1-23) min, an en bloc resection rate of 96.9%, an R0 resection rate of 50.0%, and a low incidence of adverse events (no delayed bleeding and no intra- and postoperative perforation). Moreover, UEMR also achieved good treatment outcomes: a median procedure time of 5 (range, 1-104) min, an en bloc resection rate of 82.9%, an R0 resection rate of 52.0%, and a low incidence of adverse events (delayed bleeding occurred in 2.6% of cases, and there were no incidences of no intra- and postoperative perforation). Residual recurrences occurred in two lesions (4.1%) that were treated with CSP and three lesions (4.8%) that were treated with UEMR, but these recurrences could be treated by re-endoscopic resection. Although there are limited data on these treatments for SNADETs, some previous reports and our data suggest that CSP could be indicated for adenomas sized 10 mm or less and that UEMR could be indicated for adenomas sized 10-20 mm and for intramucosal carcinomas. However, at present, the number of cases evaluated is still insufficient, and further studies are needed to evaluate long-term outcomes with enough cases.
Keywords
INTRODUCTION
The opportunities for the diagnosis and treatment of superficial nonampullary duodenal epithelial tumors (SNADETs) have been increasing, and the treatment strategy for small lesions has become a matter of concern. In the esophagus, stomach, and colon, endoscopic submucosal dissection (ESD) has been established as a relatively safe procedure that achieves a higher en bloc resection rate with negative margins compared to endoscopic mucosal resection (EMR), which reduces the local recurrence rate. However, the duodenum has the following anatomical disadvantages: it has a very thin muscular layer; there is poor operability of the endoscope; the duodenum is a retroperitoneal organ that is close to the pancreas; and there can be perioperative exposure to the bile and pancreatic juice, which causes a high incidence of complications during endoscopic resection. A previous report[1] showed that duodenal ESD has high complication rates, such as intraoperative perforation (12%), delayed perforation (4%), and delayed bleeding (4.5%). Therefore, an alternative method to ESD is desired, and that should be a reliable resection method to prevent residual recurrence as well as minimal perioperative complications. Recently, cold snare polypectomy (CSP) and underwater endoscopic mucosal resection (UEMR) have been introduced as minimally invasive treatments and are becoming more widely accepted.
We reviewed the outcomes of CSP and UEMR for SNADETs, including the results in our institution.
COLD SNARE POLYPECTOMY
In 1992, CSP was first reported by Tappero et al.[2] as “cold snare excision” for colorectal tumors; currently, its use is wide spread for the treatment of small lesions in the colon. CSP is a simple and safe endoscopic procedure that removes the lesions by mechanical strangulation of both the lesion and the normal surrounding mucosa, by using only a snare, without the use of submucosal injection or electrocautery.
CSP for colorectal polyps
CSP for colorectal polyps has already been established as one of the standard treatment options, and multiple reports have shown good treatment outcomes. Kawamura et al.[3] reported the outcomes of CSP compared with hot snare polypectomy (HSP) for the treatment of 796 sessile adenomatous colorectal polyps that were 4-9 mm in size in a multicenter randomized controlled trial (RCT). The complete resection rates for CSP and HSP were 98.2% and 97.4%, respectively, and they were proven to be non-inferior (P < 0.0001). Moreover, even in the larger subgroup of colon polyps that were 6-9 mm, the complete resection rate was 100%, suggesting that CSP could be indicated for lesions less than 10 mm in size.
A further advantage of CSP compared to HSP is a lower delayed bleeding rate. Even in the patients who underwent prophylactic clipping, comprising 81% (325/402) of the patients who had HSP and 9% (38/402) of the patients who had CSP, the delayed bleeding rate was 1.9% (4/209) for the HSP patients and 0% for the CSP patients, and the differences were significant (P = 0.02)[4].
For lesions larger than 10 mm, Murakami et al.[5] compared CSP for lesions < 10 mm versus CSP for lesions ≥ 10 mm and reported that the < 10 mm group had a significantly higher en bloc resection rate (100% vs. 93.2%, P < 0.001) and a higher histopathological complete resection rate than the ≥ 10 mm group (72.7% vs. 54.0%, P = 0.001).
Considering the above reports and referring to the American Gastroenterological Association, the European Society of Gastrointestinal Endoscopy (ESGE), and the Japanese guidelines[6-8], CSP is indicated for colorectal polyps that are nonpedunculated superficial tumors less than 10 mm in size.
CSP for SNADETs in our institution
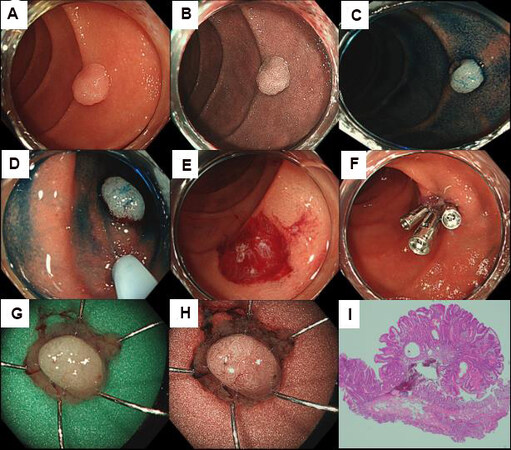
We considered CSP to be also suitable for small duodenal lesions, and it has been performed in our institution for endoscopic adenomas less than 10 mm in size since 2015[9]. The typical case treated with CSP is a 0-IIa adenoma in the Paris classification, 6 mm in size, and located in the 2nd portion. An example of this type of case is presented in Figure 1.
Figure 1. (A) Endoscopic white light image showing adenoma, 2nd portion, 0-IIa, 6 mm; (B) endoscopic narrow band imaging; (C) endoscopic image with indigo carmine spraying; (D) snaring with 10 mm snare; (E) mucosal defect after CSP with a procedure time of 1 min; (F) complete prophylactic clipping with three clips; (G) resected specimen shown as a white light image; (H) resected specimen shown by narrow band imaging; and (I) histopathological image with hematoxylin and eosin stain. The histopathological diagnosis was tubular adenoma, pHM0, pVM0.
Between January 2015 and July 2021, 64 lesions in 58 patients [male/female, 44/14; median age, 67 years (range, 39-82 years)] were resected by CSP at the Shizuoka Cancer Center. Overall, 7 lesions were in the bulbs, 55 were in the 2nd portion, and 2 were in the 3rd portion. The median size of the lesions was 6 mm (range, 2-12 mm). In total, 7 lesions had the macroscopic type of 0-I in the Paris classification, 50 were 0-IIa, 3 were 0-IIa+IIc, and 4 were 0-IIc. A preoperative biopsy was performed before CSP in 28 lesions (43.8%).
Regarding the short-term outcomes, the median procedure time (from the end of observation to the completion of resection) was 3 (range, 1-23) min. The en bloc resection rate was 96.9% (62/64). During this period, CSP was attempted for 64 lesions, but 5 lesions could not be resected without electrocautery (the CSP completion rate was 92.2%). The characteristics of the five incompletely resected lesions are described in Table 1. When the risk factors for incomplete resection were examined by evaluating predictive factors such as lesion site, gross tumor type, tumor size, availability of a preoperative biopsy, and the histopathological diagnosis, only the lesion size was found to be a statistically significant risk factor (P = 0.045, Mann-Whitney U test). However, the sample size was very small, and further investigations are needed.
Evaluation of the risk factors for incompletion of resection
| CSP completion N = 59 | CSP incompletion N = 5 | P value | |
| Location, n bulb/2nd/3rd | 6/51/2 | 1/4/0 | |
| bulb/others, n | 6/53 | 1/4 | 0.46a |
| Endoscopic size, median (range), mm | 6 (2-12) | 10 (5-10) | 0.045b |
| Macroscopic type 0-I/0-IIa/0-IIc/0-IIa+IIc | 6/47/4/2 | 1/3/0/1 | |
| with 0-IIc component/without 0-IIc, n | 6/53 | 1/4 | 0.45a |
| Biopsy before CSP | 26/59 (44%) | 2/5 (40%) | 1.00a |
| Histopathological assessment, n cancer/adenoma/non-neoplastic | 3/46/10 | 1/4/0 | |
| cancer/adenoma + non-neoplastic, n | 3/56 | 1/4 | 0.28a |
At our institution, prophylactic clipping after CSP was performed in 37 lesions (57.8%), and the percentage of spurting bleeding immediately after CSP was 0%. No adverse events or delayed complications were observed. The necessity of prophylactic clipping after CSP is controversial. Hamada et al.[10] reported no complications in patients with FAP when large numbers of polyps were resected at once without prophylactic clipping. We usually perform prophylactic clipping after CSP for the following reasons: the clipping procedure is easy because the lesions are diminutive lesions; the mucosal defects are small after CSP; and the mucosa is soft without submucosal injections.
The median size of the resected specimens was 6 mm (range, 2-22 mm), and the histopathological evaluations revealed 50 adenomas, 4 adenocarcinomas (intramucosal), and 10 nonneoplastic lesions. Of the 54 neoplastic lesions (adenomas and adenocarcinomas), the horizontal margin (HM) was negative in 27 lesions, positive in 1 lesion, and indeterminate in 26 lesions; for the vertical margin (VM), 48 lesions were negative, 1 lesion was positive, and 5 lesions were indeterminate. It has been reported that the submucosal tissue is not sufficiently resected in colorectal CSP specimens[11], and similar results might be expected in duodenal specimens. As a result, CSP could resect only the mucosal layer when using mechanical strangulation without electrocautery. Therefore, we think that CSP is inappropriate for cancers in which definitive en bloc resection is desirable because it is not able to reliably resect the submucosa and to ensure an en bloc resection with a VM0.
Regarding the long-term outcomes, 49 of 64 lesions were followed-up endoscopically for more than one month. The median observation period was 24 months (range, 1-64 months). Local recurrence was observed in 2 of 49 lesions (4.1%), which could be treated by cold forceps polypectomy or UEMR.
The advantages of CSP include a simple procedure, a short procedure time, and a low complication rate (bleeding and perforation). On the other hand, the disadvantages of CSP are the limited indications for small lesions and noncancerous lesions and a low R0 resection rate, which are common to lesions in both the colon and the duodenum.
CSP for SNADETs (other report)
Regarding the CSP for SNADETs, only one report from a single center is available. Okimoto et al.[12] reported a good long-term outcome of CSP for the treatment of sporadic SNADETs. In this report, 35 patients with SNADETs and 46 lesions were evaluated. The median lesion size was 4 mm (range, 2-7 mm); 2 lesions were located in the duodenal bulb, 40 were in the 2nd portion, and 4 were in the 3rd portion. Overall, 11 tumors were the macroscopic type 0-I in the Paris classification, 21 were 0-IIa, 12 were 0-IIa+IIc, and 2 were 0-IIc. The en bloc resection rate was 97.8%, and histopathological evaluations showed that there were 37 adenomas and 9 nontumor lesions. For the adenomatous lesions, the R0 resection rate was 70.3% (26/37), and only one lesion (2.7%) in the 36 lesions had recurrence during a median follow-up period of 48 months (3-64 months).
Comparing the short- and long-term outcomes between those of Okimoto et al.[12] and our institution [Table 2], both showed that CSP had a high rate of en bloc resection and a high rate for the completion of the procedure, with excellent long-term results, despite the low R0 resection rate, and no intra- and postoperative adverse events were observed. However, it should be noted that, although very rare, spurting delayed bleeding[13] and severe acute pancreatitis[14] as serious adverse event might occur after duodenal CSP.
Patient characteristics, procedural results (CSP), and previous literature
| (Patients/Lesions) | Our report (CSP) (58/64) | Okimoto et al.[12] (CSP) (37/46) |
| Age, median (range) | 67 (39-82) years | 68 (46-84) years |
| Sex (male/female), n | 44/14 | 24/11 |
| Location (bulb/2nd/3rd), n | 7/55/2 | 2/40/4 |
| Size (endoscopic), median (range) | 6 (2-12) mm | 4 (2-7) mm |
| Macroscopic type, n (0-I/0-IIa/0-IIa+IIc/0-IIc) | 7/50/3/4 | 11/21/12/2 |
| Biopsy before CP | 43.8% (28/64) | - |
| Closure after CP | 57.8% (37/64) | - |
| Complete resection | 92.2% (59/64) | 100% (46/46) |
| En bloc resection | 96.9% (62/64) | 97.8% (45/46) |
| Histopathological assessment, n (carcinoma/adenoma/non-neoplastic) | 4/50/10 | 0/37/9 |
| R0 resection | 50.0% (27/54) | 70.3% (26/37) |
| HMs negative | 50.0% (27/54) | - |
| VMs negative | 88.9% (48/54) | - |
| Adverse events, n delayed bleeding/intraoperative perforation/ delayed perforation | 0/0/0 | 0/0/0 |
| Recurrence | 4.1% (2/49)a | 2.7% (1/36)b |
With the above results, we believe that CSP for SNADETs should be considered for adenomatous lesions that are sized 10 mm or less. A multicenter prospective study with further long-term follow-up is currently ongoing, and the results will confirm the efficacy and safety of CSP.
UNDERWATER ENDOSCOPIC MUCOSAL RESECTION
Binmoeller et al.[15] first reported UEMR for colorectal polyps in 2012. Technically, the lesion is lifted and floated away from the muscularis propria by air deflation and water immersion; then, strangulation with mucosal and submucosal tissue is easily performed, even for flat or sessile lesions.
UEMR for colorectal polyps
A multicenter RCT[16] previously reported that UEMR significantly improved the R0 resection and en bloc resection rates compared to conventional EMR (cEMR) for colorectal polyps 10-20 mm in size [69% (59-77%) vs. 50% (40-60%), P = 0.01; 89% (81-94%) vs. 75% (65-83%), P = 0.007]. This study also showed that UEMR did not increase the incidence of adverse events. In another report[17], the local recurrence rate at the first follow-up colonoscopy was lower in tumors that were treated with UEMR than in the tumors that were treated with cEMR (7.3% vs. 28.3%, P = 0.008). A prospective RCT[18] comparing UEMR and cEMR in 20-40 mm sessile or flat colorectal polyps showed that the en bloc and R0 resection rates were 33.3% vs. 18.4% (P = 0.045) and 32.1% vs. 15.8% (P = 0.025), respectively. The results show statistical significance for the advantages of UEMR over cEMR, but both treatment outcomes were unsatisfactory. Therefore, no positive evidence is available to indicate UEMR for lesions larger than 20 mm.
There is no specific indication for UEMR in any of the guidelines of any country. To summarize the above reports, because few reports have suggested the usefulness of UEMR for lesions larger than 20 mm, the definite indication might be for lesions that are 20 mm or less. In addition, UEMR may also be effective for recurrent lesions with severe fibrosis in the submucosa[19].
UEMR for SNADETs
Binmoeller et al.[20] also reported in 2013 that UEMR could be indicated for duodenal adenomas using the same theory and technique as for the colon. UEMR for SNADETs is generally performed as follows. Firstly, the gastric and duodenal air should be deflated, and saline solution is injected through the water jet. After filling the lumen with water, resection with electrocautery is performed while making sure that the lesion is completely snared. The choice of the snare depends on the endoscopist’s preference according to the lesion characteristics (a stiff or flexible one, as well as the size of snare). Then, the specimen is grasped with forceps and removed with the scope to prevent causing the specimen to piecemeal by aspiration. Please refer to the references for the detailed procedural information[21]. Recently, a multicenter RCT that examined the safety and efficacy of UEMR for SNADETs sized 20 mm or less was reported[22]. According to the results, the outcomes of UEMR for 166 lesions in 155 patients were as follows: 50.6% (84/166) of the lesions larger than 10 mm were successfully resected, and the mean resection specimen size was 13.2 ± 5.0 mm. In total, 10 lesions were in the bulbs, 151 were in the 2nd portion, and 5 were in the 3rd portion. Overall, 18 lesions were the macroscopic type 0-I in the Paris classification, 106 were 0-IIa, and 42 were 0-IIc. The en bloc resection rate was 89.8% (149/166), and the R0 resection rate was 66.9% (111/166). The mean resection time (from the start of water immersion until the end of removal) was 5.4 ± 4.3 min, and the mean total procedure time (from the start of the water immersion until the end of closure) was 15.0 ± 8.1 min. Prophylactic clipping was achieved in 99.4% (165/166) of the cases, delayed bleeding occurred in only 1.2% (2/166) of the cases, and no perforation was observed either intra- or postoperatively. In total, 155 lesions were evaluated with a follow-up endoscopy at 12 months: 97.4% (151/155) of the lesions had no recurrence, and all four cases of recurrence were treated by re-endoscopic resection.
It is desirable to compare UEMR and conventional EMR (cEMR) as both are electric cautery and snare-based resection methods which obviously overlapped the indication. Several reports[23,24] have shown that higher en bloc and R0 resection rates were achieved with cEMR than UEMR, in contrast to the results in colorectal polyps. However, no studies have directly compared the two treatments, and RCTs comparing the two are needed to determine the indications.
UEMR for SNADETs in our institution
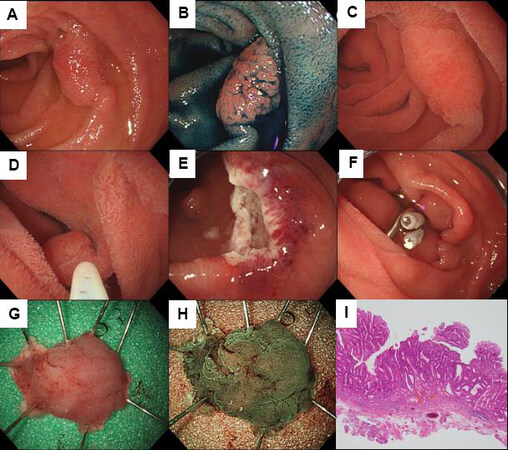
In our center, UEMR for SNADETs is indicated for adenomas larger than 10 mm and for intramucosal carcinomas no larger than 30 mm in size that are diagnosed endoscopically. The typical case treated with UEMR is an adenocarcinoma that is 0-IIa in the Paris classification, with a size of 12 mm and located in the 3rd portion. An example of this type of case is presented in Figure 2.
Figure 2. (A) An endoscopic white light image showing adenocarcinoma, 3rd portion, 0-IIa, cT1a (M), 12 mm; (B) endoscopic image showing indigo carmine spraying; (C) filling the lumen with water after air deflation; (D) snaring with 15 mm snare; (E) mucosal defect after UEMR where the procedure time was 3 min; (F) complete prophylactic clipping with two clips; (G) resected specimen shown as a white light image; (H) resected specimen shown using narrow band imaging; and (I) histopathological image by hematoxylin and eosin stain. The histopathological diagnosis was well differentiated tubular adenocarcinoma, pT1a (M), pHMX, pVM0.
Between January 2015 and July 2021 at the Shizuoka Cancer Center, 76 lesions in 71 patients [male/female: 41/30; median age: 70.5 years (range, 28-89 years)] were resected by UEMR. Overall, 12 lesions were in the bulbs, 61 were in the 2nd portion, and 3 were in the 3rd portion. The median size of the lesions was 10 mm (range, 2-40 mm). Moreover, 10 lesions were the macroscopic type 0-I in the Paris classification system, 37 were 0-IIa, 21 were 0-IIa+IIc, and 8 were 0-IIc. A preoperative biopsy was performed before UEMR in 37 lesions (48.7%).
All lesions that underwent UEMR were resected without conversion to any other techniques, such as ESD (the UEMR completion rate was 100%). The median procedure time (from the completion of water immersion to the end of resection) was 5 min (range, 1-104 min), and the en bloc resection rate was 82.9% (63/76). Compared with CSP, the en bloc resection rate of UEMR was lower, but this may be due to the invisibility of the anal side of the lesion during snaring, which could cause snare slipping. En bloc resection is ideal for an accurate pathological diagnosis; therefore, some innovations in the procedure or device are expected to solve this problem.
The percentage of spurting bleeding immediately after UEMR was 0%. Moreover, prophylactic clipping after UEMR was performed in 72 lesions (94.7%), and no intraoperative adverse events were observed. Delayed bleeding occurred in two lesions (2.6%), and no delayed perforation occurred. In both cases of delayed bleeding, the UEMR procedure was completed without prophylactic clipping, and emergency endoscopy was performed within 24 h following hematemesis. Fortunately, endoscopic hemostasis was achieved, and surgical intervention was not required. In general, resection with electrocautery is expected to suppress tumor remnants due to the “burn effect”; however, the risk of delayed bleeding increases due to microvascular damage. We believe that prophylactic clipping is an essential procedure after UEMR because of the burn effect and the larger mucosal defect in UEMR as compared with the defect in CSP, which increases the risk of postoperative complications. In addition, a previous report on colorectal polyps suggests that bipolar devices have the potential to reduce perioperative complications compared with monopolar devices, but this has not been reported in the duodenum[25].
The median size of the resected specimens was 9 mm (range, 3-40 mm). Histopathological evaluations revealed 55 adenomas, 17 adenocarcinomas (intramucosal), and 4 nonneoplastic lesions. Of the 72 neoplastic lesions (adenomas and adenocarcinomas), the HM was negative in 36, positive in 1, and indeterminate in 35; for the VM, 70 were negative, 1 was positive, and 2 were indeterminate. The R0 resection rate (en bloc resection with negative margins) was 52.0%. Similar to CSP, the R0 resection rate was relatively low. This might be due to an inadequate histopathological assessment of the specimen’s edges because the lesion is relatively small. For procedures such as UEMR and CSP, which included relatively small lesions, the R0 resection rate is an inappropriate measure for assessing the curability of endoscopic treatment, and a careful assessment of the residual recurrence rate, including the associated factors, is important.
Regarding the long-term outcomes, 52 of 76 lesions were followed up endoscopically for more than a month. Local recurrence was observed in 3 of 52 lesions (4.8%) during a median observation period of two months (range, 1-37 months). Of the three lesions with local recurrence, two lesions were treated with re-UEMR and one lesion was followed up without additional treatment due to the patient’s general condition. The procedural and long-term outcomes that were reported by Yamasaki et al.[19] and our institution are described in Table 3. A previous report and our data show that, although the R0 resection rate was low, the recurrence rate was not as high (less than 5%). Importantly, the recurrent lesions were treatable by re-endoscopic resection; however, this requires further evaluation with long-term follow-up data.
Patient characteristics, procedural results (UEMR), and previous literature
(Patients/Lesions) | Our report (UEMR) (71/76) | Yamasaki et al.[19] (UEMR) (155/166) |
| Age, median (range) | 70.5 (28-89) yearsa | 65.9 (±10.6) yearsb |
| Sex (male/female), n | 41/30 | 110/ 45 |
| Location (1st/2nd/3rd), n | 12/61/3 | 10/151/5 |
| Size (endoscopic), (range) | 10 (2-40) mma | 10.0 (±4.1) mmb |
| Macroscopic type, n (0-I/0-IIa/0-IIa+IIc/0-IIc) | 10/37/21/8 | 18/106/0/42 |
| Biopsy before UEMR | 48.7% (37/76) | 100% (166/166) |
| Closure after UEMR | 94.7% (72/76) | 99.4% (165/166) |
| En bloc resection | 82.9% (63/76) | 89.8% (149/166) |
| Histopathological assessment, n (carcinoma/adenoma/nonneoplastic) | 17/55/4 | 74/91/1 |
| R0 resection | 52.0% (39/75) | 66.9% (111/166) |
| HMs negative | 50.0% (36/72) | - |
| VMs negative | 97.2% (70/72) | - |
| Adverse events, n delayed bleeding/ intraoperative perforation/delayed perforation | 2/0/0 | 2/0/0 |
| Recurrence | 4.8% (3/52)c | 2.6% (4/155)d |
The advantages of UEMR include a relatively short procedure time and the ability to treat larger (> 10 mm) and cancerous lesions. The disadvantages of UEMR are the low R0 resection rate, which is common to lesions in both the colon and the duodenum. With the above results, we believe that the good indications of UEMR are: (1) duodenal adenomas 10-20 mm in size; and (2) intramucosal carcinomas ≤ 20 mm in size. In addition, a modified UEMR, partial submucosal injection UEMR (PI-UEMR), in which submucosal injection is performed only on the difficult side (mostly anal side), has been reported to be effective in the treatment of duodenal tumors (en bloc resection rate, 97%; R0 resection rate, 83%)[26]. An RCT of UEMR versus PI-UEMR with a primary endpoint of en bloc resection rate with pathologically confirmed negative margins without conversion to ESD (R0 resection rate) is currently underway and the results are awaited.
More cases for evaluation are needed to clarify the distinction between UEMR and other treatment methods, such as EMR or ESD.
CONCLUSION
The indications and outcomes of CSP and UEMR as minimally invasive treatments for SNADETs are outlined, and we present the results of previous reports, as well as our results. However, one of the most important problems with SNADETs was the lower preoperative diagnostic accuracy including preoperative biopsy[27-29], and further research is needed to determine whether image enhancement endoscopy is necessary and how to improve preoperative diagnostic quality. Recently, Japan and the ESGE[30,31] published guidelines on the management of duodenal tumors, which provided certain directions for the treatment of SNADETs. However, previous reports are few, and the number of cases is still insufficient; thus, further evidence is desired in the future.
DECLARATIONS
Authors’ ContributionsMade substantial contributions to the conception and design of the study, performed data analysis and interpretation, and performed data acquisition: Suwa T, Takizawa K
Availability of Data and MaterialsNot applicable.
Financial Support and SponsorshipNone.
Conflicts of InterestAll authors declare that there are no conflicts of interest.
Ethical Approval and Consent to ParticipateNot applicable.
Consent for PublicationNot applicable.
Copyright© The Author(s) 2022.
REFERENCES
1. Ono H, Kaise M, Nonaka S, et al. Clinical issues of duodenal endoscopic treatment. Stomach Intest 2016; 51:12.
2. Tappero G, Gaia E, De Giuli P, et al. Cold snare excision of small colorectal polyps. Gastrointest Endosc 1992;38:310-3.
3. Kawamura T, Takeuchi Y, Asai S, et al. A comparison of the resection rate for cold and hot snare polypectomy for 4-9 mm colorectal polyps: a multicentre randomised controlled trial (CRESCENT study). Gut 2018;67:1950-7.
4. Yamashina T, Fukuhara M, Maruo T, et al. Cold snare polypectomy reduced delayed postpolypectomy bleeding compared with conventional hot polypectomy: a propensity score-matching analysis. Endosc Int Open 2017;5:E587-94.
5. Murakami T, Yoshida N, Yasuda R, et al. Local recurrence and its risk factors after cold snare polypectomy of colorectal polyps. Surg Endosc 2020;34:2918-25.
6. Kaltenbach T, Anderson JC, Burke CA, et al. Endoscopic removal of colorectal lesions-recommendations by the us multi-society task force on colorectal cancer. Gastroenterology 2020;158:1095-129.
7. Ferlitsch M, Moss A, Hassan C, et al. Colorectal polypectomy and endoscopic mucosal resection (EMR): European society of gastrointestinal endoscopy (ESGE) clinical guideline. Endoscopy 2017;49:270-97.
8. Tanaka S, Saitoh Y, Matsuda T, et al. Evidence-based clinical practice guidelines for management of colorectal polyps. J Gastroenterol 2020;56:323-35.
9. Takizawa K, Kakushima N, Tanaka M, et al. Duodenal cold snare polypectomy (D-CSP). Stomach Intest 2016; 51:12.
10. Hamada K, Takeuchi Y, Ishikawa H, et al. Feasibility of cold snare polypectomy for multiple duodenal adenomas in patients with familial adenomatous polyposis: a pilot study. Dig Dis Sci 2016;61:2755-9.
11. Ito A, Suga T, Ota H, Tateiwa N, Matsumoto A, Tanaka E. Resection depth and layer of cold snare polypectomy versus endoscopic mucosal resection. J Gastroenterol 2018;53:1171-8.
12. Okimoto K, Maruoka D, Matsumura T, et al. Long-term outcomes of cold snare polypectomy for superficial non-ampullary duodenal epithelial tumors. J Gastroenterol Hepatol 2022;37:75-80.
13. Masunaga T, Kato M, Takatori Y. Spurting delayed bleeding on postoperative day six after cold snare polypectomy for small superficial duodenal epithelial tumor. Dig Endosc 2021;33:1198.
14. Akimoto T, Kato M, Yahagi N. Severe acute pancreatitis following cold polypectomy of the minor duodenal papilla in a case with pancreas divisum. Dig Endosc 2020;32:151.
15. Binmoeller KF, Weilert F, Shah J, Bhat Y, Kane S. “Underwater” EMR without submucosal injection for large sessile colorectal polyps (with video). Gastrointest Endosc 2012;75:1086-91.
16. Yamashina T, Uedo N, Akasaka T, et al. Comparison of underwater vs conventional endoscopic mucosal resection of intermediate-size colorectal polyps. Gastroenterology 2019;157:451-461.e2.
17. Schenck RJ, Jahann DA, Patrie JT, et al. Underwater endoscopic mucosal resection is associated with fewer recurrences and earlier curative resections compared to conventional endoscopic mucosal resection for large colorectal polyps. Surg Endosc 2017;31:4174-83.
18. Nagl S, Ebigbo A, Goelder SK, et al. Underwater vs conventional endoscopic mucosal resection of large sessile or flat colorectal polyps: a prospective randomized controlled trial. Gastroenterology 2021;161:1460-74.e1.
19. Shichijo S, Takeuchi Y, Uedo N, Ishihara R. Management of local recurrence after endoscopic resection of neoplastic colonic polyps. World J Gastrointest Endosc 2018;10:378-82.
20. Binmoeller KF, Shah JN, Bhat YM, Kane SD. “Underwater” EMR of sporadic laterally spreading nonampullary duodenal adenomas (with video). Gastrointest Endosc 2013;78:496-502.
21. Yamasaki Y, Uedo N, Takeuchi Y, et al. Underwater endoscopic mucosal resection for superficial nonampullary duodenal adenomas. Endoscopy 2018;50:154-8.
22. Yamasaki Y, Uedo N, Akamatsu T, et al. D-UEMR Study Group. Nonrecurrence rate of underwater emr for ≤ 20-mm nonampullary duodenal adenomas: a multicenter prospective study (D-UEMR study). Clin Gastroenterol Hepatol 2021:S1542-356500707.
23. Kato M, Takeuchi Y, Hoteya S, et al. Outcomes of endoscopic resection for superficial duodenal tumors: 10 years’ experience in 18 Japanese high volume centers. Endoscopy 2021; doi: 10.1055/a-1640-3236.
24. Kiguchi Y, Kato M, Nakayama A, et al. Feasibility study comparing underwater endoscopic mucosal resection and conventional endoscopic mucosal resection for superficial non-ampullary duodenal epithelial tumor < 20 mm. Dig Endosc 2020;32:753-60.
25. Shinmura K, Ikematsu H, Kojima M, et al. Safety of endoscopic procedures with monopolar versus bipolar instruments in an ex vivo porcine model. BMC Gastroenterol 2020;20:27.
26. Takatori Y, Kato M, Masunaga T, et al. Feasibility study of partial submucosal injection technique combining underwater EMR for superficial duodenal epithelial tumors. Dig Dis Sci 2022;67:971-7.
27. Kakushima N, Yoshida M, Iwai T, et al. A simple endoscopic scoring system to differentiate between duodenal adenoma and carcinoma. Endosc Int Open 2017;5:E763-8.
28. Yamasaki Y, Takeuchi Y, Kanesaka T, et al. Differentiation between duodenal neoplasms and non-neoplasms using magnifying narrow-band imaging - Do we still need biopsies for duodenal lesions? Dig Endosc 2020;32:84-95.
29. Kinoshita S, Nishizawa T, Ochiai Y, et al. Accuracy of biopsy for the preoperative diagnosis of superficial nonampullary duodenal adenocarcinoma. Gastrointest Endosc 2017;86:329-32.
30. . Japan Duodenal Cancer Guideline Committee. Clinical practice guidelines for duodenal cancer 2021. Kanehara-shuppan Pub; 2021. p. 22-31.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Suwa T, Takizawa K. Cold snare polypectomy and underwater endoscopic mucosal resection for superficial nonampullary duodenal epithelial tumors. Mini-invasive Surg 2022;6:20. http://dx.doi.org/10.20517/2574-1225.2021.123
AMA Style
Suwa T, Takizawa K. Cold snare polypectomy and underwater endoscopic mucosal resection for superficial nonampullary duodenal epithelial tumors. Mini-invasive Surgery. 2022; 6: 20. http://dx.doi.org/10.20517/2574-1225.2021.123
Chicago/Turabian Style
Suwa, Tetsuya, Kohei Takizawa. 2022. "Cold snare polypectomy and underwater endoscopic mucosal resection for superficial nonampullary duodenal epithelial tumors" Mini-invasive Surgery. 6: 20. http://dx.doi.org/10.20517/2574-1225.2021.123
ACS Style
Suwa, T.; Takizawa K. Cold snare polypectomy and underwater endoscopic mucosal resection for superficial nonampullary duodenal epithelial tumors. Mini-invasive. Surg. 2022, 6, 20. http://dx.doi.org/10.20517/2574-1225.2021.123
About This Article
Special Issue
Copyright
Data & Comments
Data

 Cite This Article 7 clicks
Cite This Article 7 clicks










Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.