Commissural alignment in TAVI: a new frontier to facilitate coronary reaccess and Redo TAVI
Abstract
As transcatheter aortic valve implantation (TAVI) expands to younger and low-risk patients with longer life expectancies, the need for post-TAVI coronary access and reintervention for failing transcatheter heart valve (THV) is expected to increase. Commissural alignment in TAVI may facilitate subsequent coronary access, avoiding severe overlap with the THV commissures, and potentially redo-TAVI. The ability to traverse a THV to access the coronary ostia is related to anatomic factors (coronary height and sino-tubular junction (STJ) height and width) and valve-related features. Furthermore, recent evidence suggests that commissural alignment after TAVI may have an impact on THV’s hemodynamics and durability. Several studies have provided technique modifications to obtain commissural alignment with available self-expanding TAVI devices. However, future efforts should aim to refine THV and delivery system designs to make neo-commissural alignment easier and safer. An individualized decision-making approach is recommended in device selection when considering future coronary access and redo-TAVI to facilitate the lifetime management of patients with aortic valve and coronary artery disease. This review aims to provide an overview of available evidence for neo-commissural alignment and strategies to achieve more anatomic valve implantation further.
Keywords
INTRODUCTION
Within the last two decades, transcatheter aortic valve implantation (TAVI) has revolutionized the treatment strategy for symptomatic severe aortic stenosis (AS), representing a less invasive alternative to surgery. Based on the results of several large-scale randomized clinical trials (RCTs), TAVI indications have now expanded from inoperable to low surgical risk patients[1,2]. As TAVI expands to younger and low-risk patients with longer life expectancies, the need for post-TAVI coronary access and reintervention for failing transcatheter heart valve (THV) is expected to increase[3]. In this context, THV orientation during initial deployment has gained importance to determine the difficulty of future coronary re-access after TAVI. Prior to recent investigations, commissural alignment of THVs appeared to be random and not reproducible during TAVI, contrary to surgical aortic valve replacement (SAVR), in which the resection of native leaflets and strict commissural alignment of bioprosthetic valves with native commissures results in no interference with coronary ostia[4].
Neo-commissural alignment during TAVI was first described by Dumonteil et al.[5] in 2013. Despite its demonstrated usefulness, then-available THVs and delivery systems did not allow interventionalists to get consistent and precise commissural alignment. The reason to aim for commissural alignment in TAVI, especially in younger patients where lifetime management becomes important, is that, with misalignment and the potential presence of a THV commissural post facing a coronary ostium, coronary access would have to be performed around the physical barrier of the commissural post. In the case of redo-TAVI evaluation, leaflet management techniques such as BASILICA cannot be performed when a commissural post faces a coronary ostium.
In light of these considerations, optimizing commissural alignment in TAVI should be pursued as this may facilitate subsequent coronary access, avoiding severe overlap with the THV commissures, and potentially redo-TAVI. This review aims to provide an overview of available evidence for neo-commissural alignment and strategies to achieve more anatomic valve implantation further.
COMMISSURAL ALIGNMENT IN TAVI: RATIONALE AND IMPLICATIONS
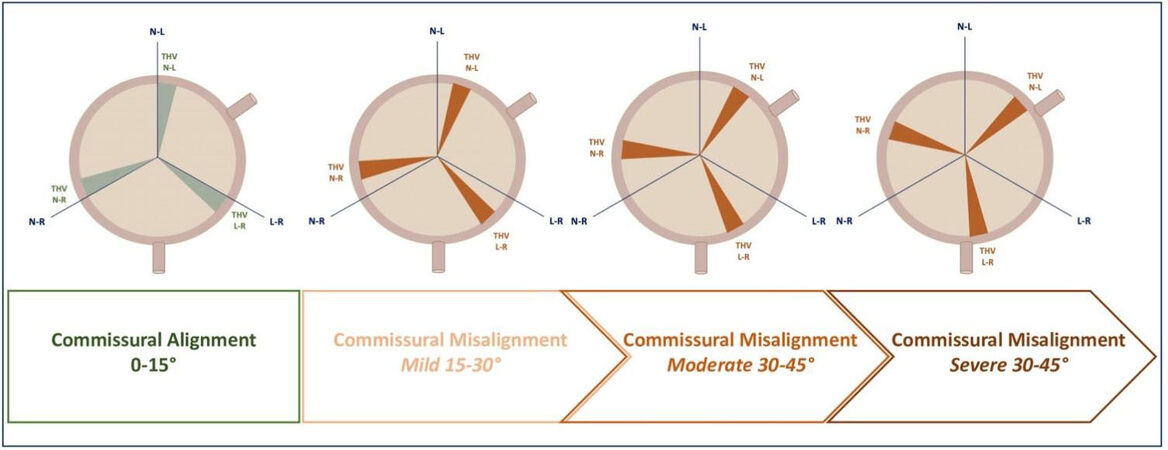
In a recent analysis, Fuchs and colleagues reported that strict alignment was obtained in only about one-fifth of patients undergoing TAVI[4]. The degree of alignment depends on the angle between coronary orifices and bioprosthetic commissures, aiming to obtain an angle between 0° and 15°. Misalignment, instead, is graded according to deviations from the native commissures in mild (from 15° to 30°), moderate (from 30° to 45°), and severe (from 45° to 60°), with coronary overlap defined as an angular distance from one of the commissural posts to a coronary ostium below 20°. The degree of misalignment is defined by the risk of overlap between neo-commissures of the THV and native coronary ostia [Figure 1]. Furthermore, despite a lack of correlation with the difference in transvalvular gradient or coronary filling, a moderate or greater commissural misalignment has been associated with a significantly higher rate of mild central aortic regurgitation[4].
Figure 1. Graphical representation of commissural alignment and different degrees of commissural misalignment following TAVI. THV: transcatheter heart valve; L-R: left-right; N-L: non-coronary-left; NRL: non-coronary-right.
RCTs comparing TAVI vs. SAVR have not reported rates of neo-commissural alignment, and available TAVI devices do not contain specific instructions. Moreover, given that aortic root and coronary anatomy differ in each patient, the development of algorithms and patient-specific implantation technique to obtain commissural alignment during TAVI would be important to improve reproducibility and ease of use.
Commissural alignment during TAVI should be achieved to facilitate future coronary access and redo-TAVI. As recently reported by Tarantini et al.[6], commissural alignment increases the feasibility of selective coronary angiography after TAVI with supra-annular devices. Furthermore, recent evidence suggests that commissural alignment after TAVI may have an impact on THV’s hemodynamics and durability. In a sub-analysis of the Low Risk TAVR trial, commissural misalignment has been associated with a higher rate of hypo-attenuated leaflet thickening (40% vs. 28%; P = 0.25)[7,8].
Coronary re-access after TAVI
The feasibility of coronary angiography and/or percutaneous coronary intervention (PCI) after TAVI was not a focus in early RCTs of high-risk and inoperable patients. The expansion of TAVI indications has undoubtedly raised the point of repeat coronary angiography and PCI due to the progressive nature of coronary artery disease and acute coronary syndromes.
In a large cohort of high-risk patients (n = 1936) enrolled in the SOURCE 3 registry treated with balloon-expandable THVs, coronary angiography was required in 3.5% of patients up to three years after TAVI, and PCI was deemed successful up to 97% of cases even in the acute setting of ST-segment elevation myocardial infarction and cardiogenic shock[9]. However, despite the advancement in THV design and procedural refinements, there is still a non-negligible risk of difficult coronary engagement after TAVI. Different factors could affect coronary re-access, including interactions between the THV and native aortic valve leaflets, being the risk of severe overlap as high as 51.4%[9,10]. Traditionally, anatomical factors, such as coronary height and STJ height and width, have been considered impactful on the ability to traverse a THV to access the coronary ostia. Moreover, THV design and its position during deployment strongly influence coronary re-engagement after TAVI. In the Reobtain Coronary Ostia Cannulation Beyond Transcatheter Aortic Valve Stent (RE-ACCESS) study, among 300 patients enrolled, unsuccessful coronary cannulation following TAVR was observed in 7.7% of cases. In this analysis, the use of self-expandable supra-annular THVs (Evolut R/PRO THVs) was associated with a higher risk of unsuccessful coronary re-access after TAVI, due to supra-annular position above the coronary ostia, the asymmetrical skirt, and closed-cell frame design. Conversely, balloon-expandable valves with their features (low-frame height, large-cell frame design, and sub-coronary implantation) facilitate coronary cannulation even when implanted in a higher position[11]. In line with this evidence, in a post-implantation computer tomography (CT) analysis, Ochiai and colleagues demonstrated that the incidence of CT features of unfavorable coronary access (coronary ostium located below the skirt or in front of the THV commissural posts above the skirt) occurred more frequently in the Evolut R/Evolut PRO group than the SAPIEN 3 group (left coronary artery (LCA) 34.8% and right coronary artery (RCA) 25.8% vs. LCA 15.7% and RCA 8.1%, respectively)[12].
Among the most important factors influencing coronary re-access with the use of a self-expanding valve, we have to include implantation depth. Recently, an implantation depth of at least 4 mm below the annular plane has been advised to avoid an overlaying between the skirt, theoretically designed to prevent paravalvular regurgitation, and coronary arteries.
Yudi et al.[13] proposed an algorithm to guide interventional cardiologists in the engagement of coronary ostia after TAVI, advising the use of a smaller catheter for the left coronary artery (JL 3.5 and JL 3 for femoral and radial access) or the Ikari right guide catheter for self-expanding THVs, without significant technical changes in the presence of balloon-expandable valves.
Strong efforts should be directed toward valve selection and commissural alignment to achieve more anatomic valve implantation and better preserve coronary access. Careful consideration should be reserved to patients with low coronary height at the time of valve selection and implantation, not only to avoid dreadful complications, such as acute coronary occlusion, but also to allow easy coronary re-engagement, specifically important in the management of eventual acute coronary syndrome when rapid revascularization is crucial.
Redo-TAVI
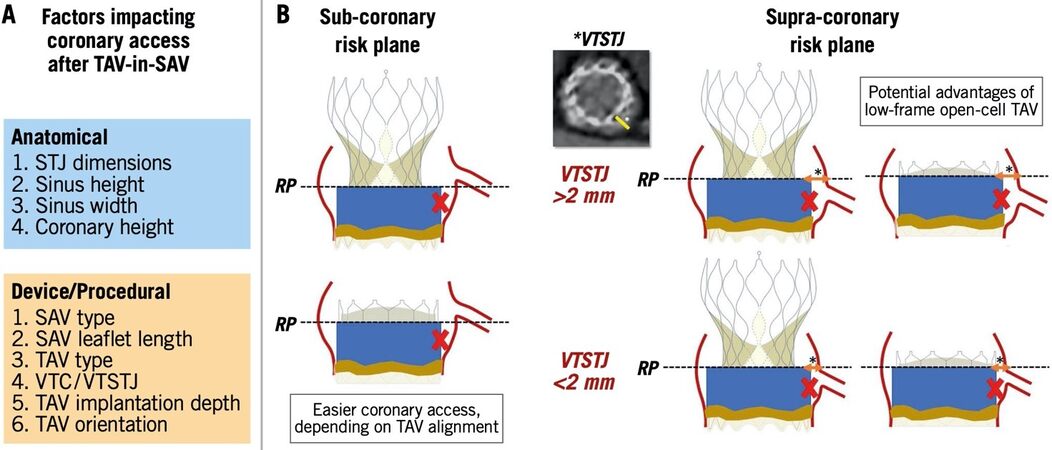
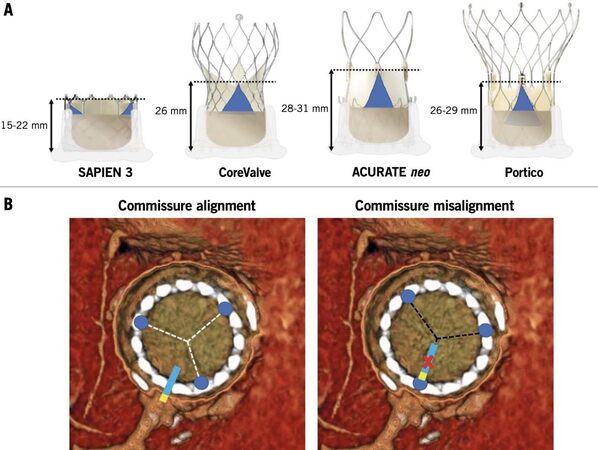
In the last few years, given the likelihood of structural valve deterioration and non-structural valve dysfunction after index TAVI, redo-TAVI has emerged as a therapeutic alternative to TAVR-explant in anatomically suitable patients[14]. Better outcomes over time for redo-TAVI have been mainly driven by improved patient selection and procedural techniques leading to a lower rate of valve malpositioning and coronary obstruction. However, redo-TAVI carries a non-negligible risk of acute coronary obstruction [3.5% reported in Valve-in-Valve International Data (VIVID) registry], differently from redo-SAVR, where commissural alignment between surgical and native valve is easily obtained. Moreover, the vertical displacement of the first THV after redo-TAVI, in addition to the native aortic valve leaflets, makes coronary access after redo-TAVI even more challenging due to the risk of sinus of Valsalva sequestration[15]. This complication occurs more frequently with self-expandable THVs, as demonstrated in RESOLVE registry where Evolut R/Evolut PRO platforms carried a significantly higher risk of sinus sequestration compared to the SAPIEN 3 valve (45.5% vs. 2.0%; P < 0.001, respectively) because of Evolut’s supra-annular leaflets and tall commissural height[16]. Tarantini et al.[17] proposed an algorithm on TAVI vs. SAVR at the index aortic valve intervention based on the STJ anatomy to evaluate the risk of coronary re-access after redo-TAVI. Anatomical, device, and procedural factors affecting coronary access after redo-TAVI in prostheses with a sub-coronary or supra-coronary risk plane are provided in Figure 2. Tall-frame THV have higher asymmetric commissures, as shown in Figure 3, thus making the use of low-frame THV advantageous for redo-TAVI.
Figure 2. Factors impacting coronary access after redo-TAVI in prostheses with a sub-coronary or supra-coronary risk plane. (A) Factors impacting coronary access after TAV-in-SAV. (B) Sub-coronary risk plane and supra-coronary risk plane. RP: risk plane; SAV: surgical aortic valve; TAV: transcatheter aortic valve; VTC: virtual transcatheter heart valve to coronary distance; *means VTSTJ; VTSTJ: virtual transcatheter heart valve to sinotubular junction distance. From Tarantini et al.[14] (permission for publication obtained).
Figure 3. Impact on coronary access of misaligned high THV commissural posts: (A) commissure height of different transcatheter heart valves; and (B) examples of neo-commissure alignment versus misalignment with the native coronary ostia. From Tarantini et al.[14] (Permission for publication obtained).
Commissural alignment is also of the utmost importance during initial TAVI as misalignment makes any leaflet management strategy such as BALISICA (bioprosthetic or native aortic scallop intentional laceration to prevent iatrogenic coronary artery obstruction) difficult or unfeasible. This technique has been successfully applied in TAVI-in-SAVR procedures, but its use in TAVI-in-TAVI is possible only when commissures of the first THVs are aligned with the natives[18]. Moreover, in the setting of TAVI-in-TAVI other protective strategies, such as chimney stenting (preemptive positioning of stent and deployment in obstructive coronary ostium), may not be useful because the stent frames in the aortic root are covered by first TAVI leaflets.
Given these considerations, in redo-TAVI, a tailored screening on the risk of coronary obstruction is strongly recommended. It should be carefully performed in each patient and achieved through dedicated pre-procedural CT and fluoroscopic imaging analysis.
ACHIEVING COMMISSURAL ALIGNMENT WITH DIFFERENT THV TYPES
Patient-specific alignment of TAVI devices is nowadays allowed by pre-procedural CT analysis, performed not only to identify the coplanar implant view but also to add anatomical information about coronary ostia orientation and native commissures. CT-based commissural alignment can be planned, aiming to identify specific fluoroscopic projection or predicting TAVI system axial rotation. The Alignment of Transcatheter Aortic-Valve Neo-Commissures (ALIGN TAVR) study first evaluated the impact of initial THV deployment orientation on neo-commissural overlap with coronary arteries[19,20]. Afterwards, other studies have extensively addressed this issue.
In this section, we provide a summary of available data for the main types of TAVI devices.
Self-expanding THVs
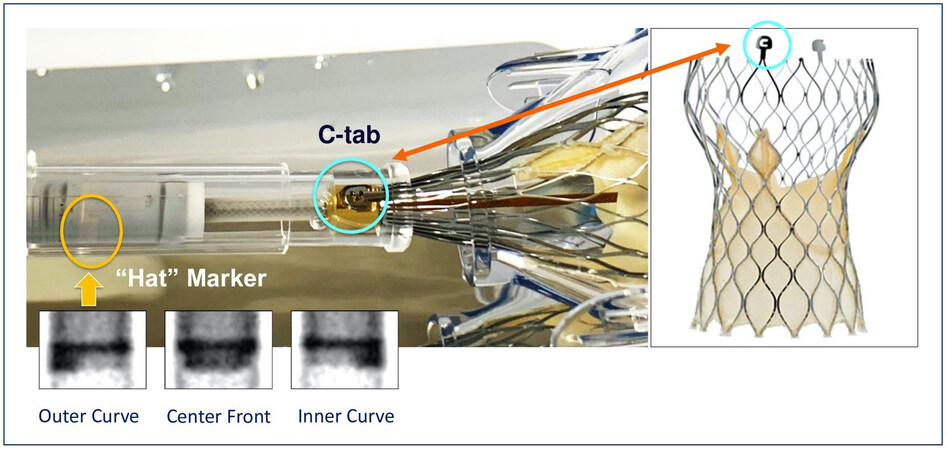
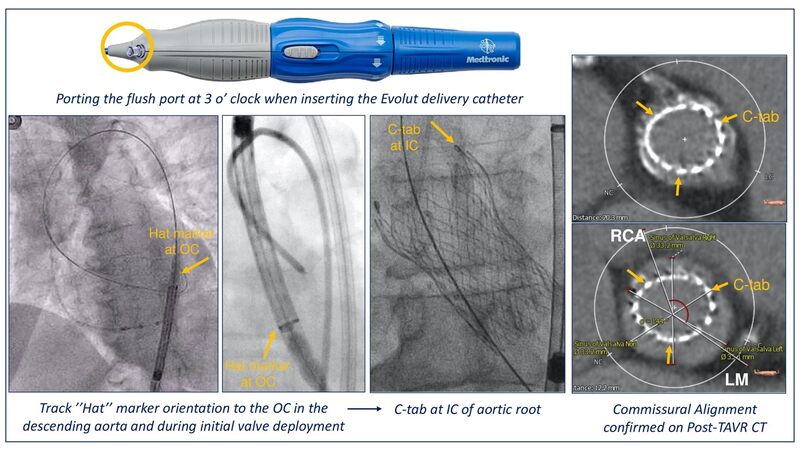
The importance of commissural alignment during self-expandable THV implantation is highlighted above. In the ALIGN TAVR study, 828 TAVR implants (SAPIEN 3, 483; Evolut, 245; ACURATE-neo, 100) were analyzed using pre-procedural multidetector row CT and coplanar fluoroscopy coregistration. Significantly less severe coronary overlap was obtained according to the precise positioning of the Hat marker of CoreValve Evolut that can be oriented in one of four positions: anterior or posterior in the center of the deployment device [center front (CF) or center back (CB)] or in the inner (IC) or outer curve (OC) of the aortic annulus [Figure 4].
A Hat marker is a radiopaque marker at the distal part of the delivery catheter, located at an angle of 90° to the right from the C-tab, that is aligned with one of the commissures and with the flush port. Evolut Hat position at OC or CF during initial deployment improved commissural alignment and reduced the rate of coronary artery overlap (from 36% to 60%; P < 0.05) compared to Hat marker positioned toward the IC or CB. Furthermore, the best rate of right orientation of the Hat marker was obtained positioning Evolut flush port at 3 o’clock [Figure 5][21]. This maneuver can be performed during initial insertion in the femoral artery as the rotation of the delivery system is limited inside the patient, given there are two spines within the Evolut catheter. In fact, we accumulated over 450 consecutive case experiences with the Evolut THV platform using this insertion technique from March 2019 and from January 2020 to July 2021. Among 316 Evolut TAVI cases, we were able to get the Hat position to the outer curve or center front 96.8% of the time. However, some limitations regarding flush port positioning have been reported: other approaches different from transfemoral access have not been studied, and tortuosity and calcification of the ileo-femoral axis could reduce the ability of Hat marker orientation.
Figure 5. Commissural alignment with the Evolut system. Tang et al.[20] (Permission for publication obtained).
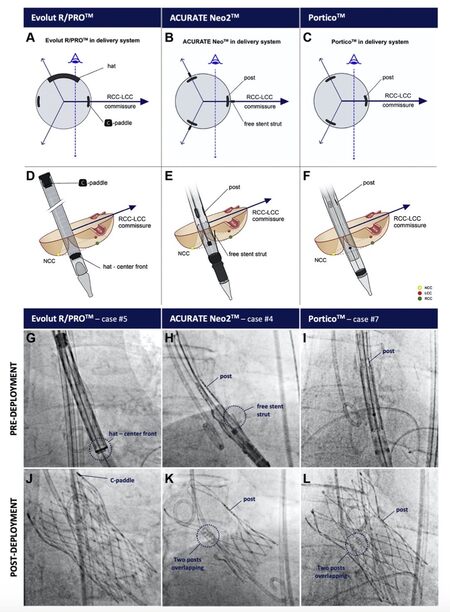
Patient- and device-specific implantation techniques were evaluated by Bieliauskas et al.[22] in an analysis of 60 consecutive patients treated with three different self-expanding THV platforms (Evolut, 20; Acurate-neo2, 20; Portico, 20). The authors obtained optimal commissural alignment in 60% of cases with equal or less than mild misalignment in 88% of cases. Specifically, for all three platforms, the same implantation sequence was followed. After inserting the system with a flush port at 3 o’clock for Evolut, 6 o’clock for Acurate, and 12 o’clock for Portico, the valve was positioned at the level of the anulus in a cusp overlap view. Then, the THV orientation was assessed and, if needed, a slow rotation of delivery catheter was performed to obtain a CF position of the Hat marker for Evolut or to isolate on the right one of the THV markers for Acurate and Portico[22].
Whenever possible, the Hat marker of the Evolut valve should be oriented in the descending aorta before tracking across the aortic arch and valve deployment. Indeed, the position of neo-commissures can be predicted by Hat mark orientation resulting in an anterior 90° angle position of the C-tab with respect to both coronary ostia during valve deployment. This position of valve neo-commissures may allow easier coronary re-access[23]. Furthermore, in cases where the center angle projection is difficult to obtain, a lateral approach has been described, using a CT projection where two coronaries were visible in the same plane and its orthogonal plane[24]. An illustration of how the radiopaque THV commissural markers should be oriented in the cusp overlap view for each of the three different self-expanding valves (Evolut R/PRO, Acurate Neo2 and Portico) is provided in Figure 6.
Figure 6. THV-specific instructions for implantation in RCC/LCC cusp overlap view to achieve neo-commissural alignment. Illustration of how the radiopaque THV commissural markers should be oriented in a transversal plane (A-C) and from a fluoroscopic perspective using the RCC/LCC cusp overlap view (D-F) in order to obtain neo-commissural alignment-and this for the Evolut R/PRO (left column), ACURATE neo2 (middle column), and Portico valve (right column) (G-L). From Bieliauskas et al.[22] (Permission for publication obtained).
Patient-specific commissural alignment of the self-expanding Evolut valve using the cusp overlap view has also been described in 13 consecutive ViV procedures with successful valve implantation in all patients and well-aligned commissures in 95% of cases at post-procedural CT scan[25].
Even though the evidence from these studies provides technique modifications to obtain commissural alignment with available self-expanding TAVI devices, further improvements in THV and delivery system design are ultimately needed.
Balloon-expandable THVs
Crimping one commissure at 3, 6, 9, or 12 o’clock can change initial deployment orientation for balloon-expandable THV. Differently from self-expandable valves, no improvement in commissural alignment was observed in the ALIGN TAVR study with different crimping of the SAPIEN 3 THV[20]. This is usually less impactful on future coronary re-access given the design of the SAPIEN 3 valve with low frame height and large-cell frame. Diagnostic and therapeutic angiography can easily be performed cannulating coronary ostia above the top of the stent frame. The unique challenging scenario is represented by cases in which SAPIEN 3 protrudes above narrow STJ[16].
However, achieving commissural alignment can have a beneficial effect on long-term stress on prosthetic leaflets, improving hemodynamics, including when a balloon-expandable valve is implanted. For these reasons, a recent study has described a novel method of assessing commissural alignment for SAPIEN 3 based on pre-procedural 3D-CT and fluoroscopy in two views[26]. Despite some limitations, this method could be employed in larger studies to evaluate the impact of misalignment of valve durability and clinical outcomes.
Mechanically expandable LOTUS THVs
Despite the increased awareness of the importance of future coronary re-access after TAVI, no data exist about commissural alignment with mechanically expandable LOTUS valves. The cylindrical shape strongly influences the interaction between THV flame and native STJ. Indeed, Moriyama et al.[27] reported a high rate of unfavorable coronary access (29.3% for LCA and 41.5% for RCA) with Lotus THV, mainly because only two pathways, “above the THV flame” and “through outside of the THV flame”, were available for achieving selective coronary cannulation after TAVI.
FUTURE DIRECTIONS
In contemporary TAVI practice, optimal valve selection and implantation techniques have achieved better procedural outcomes. However, further efforts should aim to refine THVs design and delivery system to make neo-commissural alignment easier and safer to facilitate the lifetime management of patients with aortic valve and coronary artery disease[28,29]. Different principles should guide the design of future THVs: (1) a leaflet posts position easily identified on fluoroscopy; (2) the possibility of an easy and safe rotation of delivery system across the aortic valve reducing the risk of aortic damage; and (3) specific instructions to align bioprosthetic valve commissures with the native provided by the manufactures. Available evidence sheds light on the features of the ideal device to ensure optimal long-term outcomes in terms of valve hemodynamic and durability, eventual future coronary access, and/or ViV procedures.
CONCLUSIONS
Given the increasing number of younger patients with severe AS undergoing TAVI, the number of patients requiring coronary angiography and/or PCI as well as redo-TAVI is expected to increase. Therefore, preserving a manageable coronary re-access after TAVI is becoming a priority in the management of these patients. The ability to traverse a THV to access the coronary ostia is related to anatomic factors (coronary height, STJ height, and width) and valve-related features. Self-expanding platforms may present technical challenges due to their supra-annular position above the coronary ostia, closed-cell frame design, and asymmetrical skirt. Modified delivery system insertion techniques have been linked to better commissural alignment and less coronary overlap with self-expandable THVs, but further studies are needed to confirm and improve their reproducibility. Conversely, balloon-expandable valves, given their low frame height with sub-coronary implantation and large-cell frame design, generally ensure easier coronary ostium cannulation despite commissural misalignment. However, commissural alignment is helpful in all THV platforms for redo-TAVI, especially when the risk plane is above the coronary ostia and even STJ, risking sinus sequestration and coronary obstruction with redo-TAVI. An individualized decision-making approach is recommended in device selection and sizing when considering future coronary access and redo-TAVI.
DECLARATIONS
Author contributionsDrafted and revised the manuscript: Avvedimento M
Drafted and revised the manuscript and approved the final manuscript: Tang GHL
Availability of data and materialsNot applicable.
Financial support and SponsorshipNone.
Conflict of InterestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2022.
REFERENCES
1. Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA Guideline for the management of patients with valvular heart disease: executive summary: a report of the american college of cardiology/american heart association joint committee on clinical practice guidelines. Circulation 2021;143:e35-71.
2. Vahanian A, Beyersdorf F, Praz F, et al. ESC/EACTS Scientific Document Group. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 2022;43:561-632.
3. Avvedimento M, Tang GHL. Transcatheter aortic valve replacement (TAVR): recent updates. Prog Cardiovasc Dis 2021;69:73-83.
4. Fuchs A, Kofoed KF, Yoon SH, et al. Commissural alignment of bioprosthetic aortic valve and native aortic valve following surgical and transcatheter aortic valve replacement and its impact on valvular function and coronary filling. JACC Cardiovasc Interv 2018;11:1733-43.
5. Dumonteil N, Marcheix B, Lairez O, Laborde JC. Transcatheter aortic valve implantation for severe, non-calcified aortic regurgitation and narrow aortic root: description from a case report of a new approach to potentially avoid coronary artery obstruction. Catheter Cardiovasc Interv 2013;82:E124-7.
6. Tarantini G, Nai Fovino L, Scotti A, et al. Coronary access after transcatheter aortic valve replacement with commissural alignment: The ALIGN-ACCESS Study. Circ Cardiovasc Interv 2022;15:e011045.
7. Salmonsmith JA, Ducci A, Burriesci G. Does transcatheter aortic valve alignment matter? Open Heart 2019;6:e001132.
8. Khan JM, Rogers T, Weissman G, et al. Anatomical characteristics associated with hypoattenuated leaflet thickening in low-risk patients undergoing transcatheter aortic valve replacement. Cardiovasc Revasc Med 2021;27:1-6.
9. Tarantini G, Nai Fovino L, Le Prince P, et al. Coronary access and percutaneous coronary intervention up to 3 years after transcatheter aortic valve implantation with a balloon-expandable valve. Circ Cardiovasc Interv 2020;13:e008972.
10. Tang GHL, Zaid S, Ahmad H, Undemir C, Lansman SL. transcatheter valve neo-commissural overlap with coronary orifices after transcatheter aortic valve replacement. Circ Cardiovasc Interv 2018;11:e007263.
11. Barbanti M, Costa G, Picci A, et al. Coronary cannulation after transcatheter aortic valve replacement: the re-access study. JACC Cardiovasc Interv 2020;13:2542-55.
12. Ochiai T, Chakravarty T, Yoon SH, et al. Coronary access after TAVR. JACC Cardiovasc Interv 2020;13:693-705.
13. Yudi MB, Sharma SK, Tang GHL, Kini A. Coronary angiography and percutaneous coronary intervention after transcatheter aortic valve replacement. J Am Coll Cardiol 2018;71:1360-78.
14. Tarantini G, Dvir D, Tang GHL. Transcatheter aortic valve implantation in degenerated surgical aortic valves. EuroIntervention 2021;17:709-19.
15. Tang GHL, Zaid S. Coronary re-access after redo TAVI: a proposed classification to simplify evaluation. EuroIntervention 2020;16:e960-2.
16. Ochiai T, Oakley L, Sekhon N, et al. Risk of coronary obstruction due to sinus sequestration in redo transcatheter aortic valve replacement. JACC Cardiovasc Interv 2020;13:2617-27.
17. Tarantini G, Nai Fovino L. Coronary access and TAVR-in-TAVR: don't put off until tomorrow what you can do today. JACC Cardiovasc Interv 2020;13:2539-41.
18. Khan JM, Babaliaros VC, Greenbaum AB, et al. Preventing coronary obstruction during transcatheter aortic valve replacement: results from the multicenter international BASILICA registry. JACC Cardiovasc Interv 2021;14:941-8.
19. Tang GHL, Zaid S, Gupta E, et al. Impact of initial evolut transcatheter aortic valve replacement deployment orientation on final valve orientation and coronary reaccess. Circ Cardiovasc Interv 2019;12:e008044.
20. Tang GHL, Zaid S, Fuchs A, et al. Alignment of transcatheter aortic-valve neo-commissures (ALIGN TAVR): impact on final valve orientation and coronary artery overlap. JACC Cardiovasc Interv 2020;13:1030-42.
21. Tang GHL, Sengupta A, Alexis SL, et al. Conventional versus modified delivery system technique in commissural alignment from the Evolut low-risk CT substudy. Catheter Cardiovasc Interv 2022;99:924-31.
22. Bieliauskas G, Wong I, Bajoras V, et al. Patient-specific implantation technique to obtain neo-commissural alignment with self-expanding transcatheter aortic valves. JACC Cardiovasc Interv 2021;14:2097-108.
23. Fabris E, Vitrella G, Rakar S, Perkan A, Bedogni F, Sinagra G. Hat-marker orientation to minimize neo-commissural overlap with coronaries during corevalve evolut TAVR. JACC Cardiovasc Interv 2020;13:782-3.
24. Takamatsu M, Fuku Y, Ohya M, Shimamoto T, Komiya T, Kadota K. Lateral approach for modifying hat-marker orientation to minimize neo-commissural overlap during transcatheter aortic valve replacement. JACC Cardiovasc Interv 2020;13:e199-201.
25. Kitamura M, Wilde J, Dumpies O, et al. Patient-specific neocommissural alignment of the evolut valve: a pilot study in transcatheter aortic Valve-in-Valve replacement. JACC Cardiovasc Interv 2021;14:934-6.
26. Spilias N, Sabbak N, Harb SC, et al. A novel method of assessing commissural alignment for the SAPIEN 3 transcatheter aortic valve. JACC Cardiovasc Interv 2021;14:1269-72.
27. Moriyama N, Shishido K, Yokota S, et al. Coronary access after TAVR with a cylindrical shaped valve: Learning from LOTUS. Cardiovasc Revasc Med ;2021:S1553-8389(21)00273.
28. Tang GHL, Zaid S. Commissural alignment using cusp-overlap view in self-expanding TAVR: a step closer to achieving surgical-like orientation? JACC Cardiovasc Interv 2021;14:2109-11.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Avvedimento M, Tang GHL. Commissural alignment in TAVI: a new frontier to facilitate coronary reaccess and Redo TAVI. Mini-invasive Surg 2022;6:24. http://dx.doi.org/10.20517/2574-1225.2021.143
AMA Style
Avvedimento M, Tang GHL. Commissural alignment in TAVI: a new frontier to facilitate coronary reaccess and Redo TAVI. Mini-invasive Surgery. 2022; 6: 24. http://dx.doi.org/10.20517/2574-1225.2021.143
Chicago/Turabian Style
Avvedimento, Marisa, Gilbert H. L Tang. 2022. "Commissural alignment in TAVI: a new frontier to facilitate coronary reaccess and Redo TAVI" Mini-invasive Surgery. 6: 24. http://dx.doi.org/10.20517/2574-1225.2021.143
ACS Style
Avvedimento, M.; Tang GHL. Commissural alignment in TAVI: a new frontier to facilitate coronary reaccess and Redo TAVI. Mini-invasive. Surg. 2022, 6, 24. http://dx.doi.org/10.20517/2574-1225.2021.143
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 32 clicks
Cite This Article 32 clicks











Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.