Uniportal thoracoscopic decortication: start away from empyema approach
Abstract
Aim: Video-assisted thoracoscopic surgery (VATS) is now a gold standard in treating early-stage empyema, while much debate still exists considering the effectiveness of this approach for late-stage empyema. Most concerns arise from the crowded rib cage, narrow working space, and ability to free trapped lungs quickly, mainly if uniportal VATS is used. However, unlike uniportal VATS lobectomy, there is no consensus about standard steps for uniportal VATS decortication to ensure smooth and effective surgery. We try to offer standard, easy-to-replicate steps for this approach to evaluate the efficacy and safety of the “start away from empyema” approach for uniportal VATS decortication in the management of stage II and III empyema.
Methods: A prospective case series study has been conducted on 25 patients. All patients with stage II and III empyema were admitted to the Cardiothoracic Surgery Department between October 2017 and March 2020. VATS procedure was done under general anesthesia by a double-lumen tube for selective ventilation. Demographic data, preoperative diagnosis, intraoperative findings, hospital stay, and complications were recorded.
Results: Twenty-five patients were enrolled in this study with a median age of 35 years. The duration of illness ranged between 14 and 60 days, with a median (IQR) of 25 (17) days. In (88%) of the patients, there was a successful outcome defined as a near-complete resolution on Chest X-ray (scoring of 3 or 4) and chest US (scoring of 2 or 3). Only three (12%) patients had a partially successful outcome. All patients with partial success suffered from infection associated with malignant effusion.
Conclusion: “Start away from empyema” approach for uniportal VATS decortication in stage II and III empyema could be safe and effective in treating loculated nonmalignant pleural effusion.
Keywords
INTRODUCTION
Despite the rapid pace in the field of minimally invasive thoracic surgery, mainly uniportal VATS, many centers do not adopt this technique for late-stage empyema. The main concerns are narrow working space, crowded ribs, and a long learning curve. Nevertheless, the incidence of empyema has increased during the last years as the annual rate was 7.15 cases per 100,000 inhabitants in 2013 and increased to 7.75 cases per 100,000 inhabitants in 2017. In the most recent reports, mortality has exceeded 10% in parapneumonic empyema[1]. VATS debridement is a well-established approach for early-stage empyema. However, there are no standard steps for VATS decortication, especially when doing uniportal VATS decortication.
Starting from the empyema pouch, as Bongiolatti et al.[2] described, has many difficulties. The pouch site is mainly the narrowest part of the chest cavity with crowded ribs.
Moreover, it is always tricky not to injure the underlying lung as a surgeon cannot see through thick pleura. Furthermore, extensive adhesions between the empyema pouch and chest wall make no space for proper dissection to detect the proper decortication plan accurately. Therefore, we develop the “Start Away From Empyema” technique to position the single port at the classic position of the fifth intercostal space just anterior to the anterior axillary line, empyema pouch, or loculations are usually found posterior and towards the diaphragm. By starting at that point, we assume that we are away from the empyema pouch in a non-dependent area where we can sweep the lung down and get more space to work in before approaching the empyema pouch. Nevertheless, this will enhance the ability to protect the lung from accidental injury during the dissection of thick peel.
We aimed to evaluate the Start Away From Empyema (SAFE) uniportal VATS decortication in managing patients with empyema and determining predictors of success among studied patients.
METHODS
A prospective case series study was conducted on 25 patients. All patients with stage II and III empyema were admitted to Cardiothoracic Surgery Department during the period between October 2017 and March 2020.
Inclusion criteria
According to Yang et al.[6] classification, a patient diagnosed with stage II and III empyema by chest imaging and ultrasound.
Patients with difficult pleural fluid drainage 24 hours after non-VATS procedures such as intercostal tube (ICT) or medical thoracoscopy provided that the tube was correctly positioned and patent. The patient agreed to contribute to this study and was fit for general anesthesia.
Exclusion criteria
If one of the following criteria met, the patient was excluded:
• Patients who were not expected to get a value after drainage of the pleural fluid.
• A patient was not fit for general anesthesia.
• A patient refused to be included in this study.
All included patients were subjected to the following:
1. Complete medical history and clinical examination.
2. Investigations to evaluate patient fitness for general anesthesia.
3. Chest X-ray and CT scan before the procedure and serial follow-up with chest X-ray until tube removal.
Chest ultrasonography was conducted by a well-trained chest physician (specialist level), and the results were verified by a consultant chest physician in the Ultrasound Unit at Chest Department via the apparatus (ALOKA - Prosound - SSD - 3500SV). Intrapleural adhesions were classified according to Yang et al.[6] into:
1. Anechoic
2. Complex non-septated effusion
3. Complex septated pleural effusion
4. Homogenous echogenic
Treatment protocol
VATS was done under general anesthesia, using a double-lumen tube and lung isolation. This work was performed in the cardiothoracic surgery operative room. The institutional ethical committee approved the study, and the clinical trial was registered (ClinicalTrials.gov Identifier: NCT03172052) with the informed consent obtained.
• A small incision (up to 3 cm) was made in the fifth intercostal space at the anterior axillary line, dissection of the subcutaneous tissue and muscles was done. In most cases, no trocar was used, but in obese patients, a soft tissue retractor was used. A 30-degree lens (Karl-Storz) in a 10-mm sheath thoracoscopy was introduced at the topmost of the incision. Instruments were inserted below the thoracoscopy lens. We swept the lung down via the tip of suction or sponge on a stick, which was usually adherent to the chest wall by some degree until we could see the thick pleural and decorticate it from the lung while the empyema pouch was kept intact. After exposing the pouch, we opened the empyema pouch, evacuating all fluid contents using suction and a 50-cc syringe for sampling. Dense pus contents and biofilm were removed by oval or nodal grasping forceps. Irrigation with warm saline was then performed [Figure 1]. Thoracoscopic debridement was completed with drainage of all pus and breakage of adhesions.
Figure 1. Operative steps of uniportal VATS decortication; SAFE approach. VATS: Video-assisted thoracoscopic surgery; SAFE: Start Away From Empyema.
• Thoracoscopic decortication was completed by removing thick peel resembling the wall of empyema pouch via blunt dissection by the tip of suction or sponge on a stick on the lung surface counteracted by grasping forceps holding the thick peel. The fissures were opened by blunt and sharp dissection, peel over the diaphragm was removed, and the parietal pleura overlying the chest wall was left.
• After performing decortication, warmed saline was irrigated again inside the pleural cavity through a 50-cc syringe, then suctioned after the anesthetist started to ventilate the lung and check for air leak. Hemostasis was achieved by compression and electrocautery. Sealants managed to control air leakage for small visceral leaks and sutures for large tears.
• We considered decortication was completed when full lung expansion occurred (lung expanded till chest wall or less than 1 cm from the chest wall) with the anesthetist delivering pressure between 30 and 35 mmHg to the lung. The decortication was revised if the lung failed to be fully expanded. The operator had the option to either continue VATS or convert to open surgery.
• One chest tube (size 28-32 Fr.) was inserted from the same opening, and the rest of the port was closed in layers.
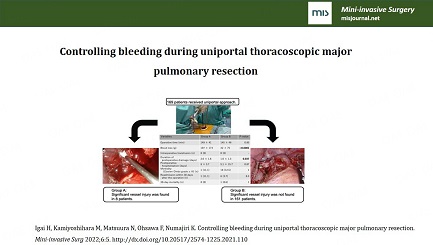
Supplementary Video 1 demonstrated the procedural steps to achieve the hemostasis after the middle lobe of the pulmonary artery just behind the bronchus was injured by tip of the stapler during uniportal thoracoscopic middle lobectomy.
The effectiveness of protocol was assessed by:
1 - Chest X-ray to confirm radiological clearance by comparing the first with the last chest X-ray taken on discharge.
2 - Chest ultrasound to confirm the dissolution of adhesions.
Chest X-ray was scored on the discharge into:
0 - No change in the first X-ray before VATS.
1 - Less than 1/3 improvement/lung expansion.
2 - Improvement between 1/3 and 2/3.
3 - More than 2/3 improvement without complete clearance of effusion.
4 - Complete radiological clearance/complete lung expansion.
Chest US findings were scored at the discharge into:
0 - No change.
1 - Dissolution of adhesions in some regions.
2 - Dissolution of adhesions in all regions with residual pleural affection.
3 - Total adhesion dissolution without residual pleural lesion.
Assessment of the outcomes:
Failure: Chest X-ray scoring 0, and chest US scoring 0.
Partially successful: Chest X-ray scoring 1 or 2 and chest US scoring 1.
Successful: Chest X-ray scoring 3 or 4, and chest US scoring 2 or 3.
The duration of hospital stay for included patients was recorded from the day the patient was operated on until the day the procedure’s success was accessed. In successful cases, the intercostal tube was removed, and the patient was discharged to continue specific treatment according to the underlying pathology.
Complication assessment
Patients were assessed for complications. Fever was defined as a temperature greater than 38C, or one-degree elevation over baseline in previously febrile patients. Also, the complications included minor or significant bleeding for which blood transfusion was requested and pain assessed using a color analog scale, with red representing severe pain, yellow representing moderate pain, and green representing comfort.
Statistical analysis
Data were analyzed using the computer software program SPSS software package version 21. Descriptive statistics were performed with frequency, cross-tabulations for categorical variables, and median (IQR) for quantitative data. The chi-square test was used for comparing independent categorical variables, and Mann Whitney and Wilcoxon tests were used for dichotomous groups for quantitative data as it was not normally distributed. P-values less than 0.05 were considered significant.
RESULTS
Twenty-five patients (15 males and ten females) with a median age of 35 years and a range between 22 and 63 years old were included. The duration of illness ranged between 14 and 60 days, with the median (IQR)duration being 25 (17) days. A median number of previous aspirations was one with a range between one and two [Table 1].
Descriptive data of the empyema patients subjected to the SAFE approach
| Studied patients (n = 25) | ||
| Age (years) | ||
| Median | 35 | |
| Range | 22-63 | |
| Sex | Male | 15 (60.0%) |
| Female | 10 (40.0%) | |
| Duration of illness (days) | ||
| Median | 25 | |
| IQR | 17 | |
| Previous aspiration | ||
| Median | 1 | |
| IQR | 0 | |
| Empyema stage | Stage II (Yang 2&3) = 20 Stage III (Yang 4) = 5 | |
The most frequent underlying etiology among studied patients was bacterial empyema thoracis (60%) followed by tuberculous effusion (28%). In three infected patients (12%), malignant effusion was present. The drained amount of the fluid was significantly increased after VATS [with median (IQR) 200 (400) before VS, 1800 (1000) after (ml); P < 0.001].
The majority of patients in the studied group (88%) (n = 25) had a successful outcome. Only three patients (12%) had a partially successful outcome. Although the duration of illness was insignificant, it was longer among the patients with partial success [50 (29) compared with 23 (13.25) days; P = 0.08]. All patients with partial success had underlying malignant effusion, while patients with successful outcomes had empyema and tuberculous effusion [Figure 2]. All patients with successful outcomes got a clinical improvement and did not need another intervention or surgery during a follow-up period of one year. Patients with partial improvement got radiological improvement but did not get the full lung expansion, and one patient continued to complain of fever after discharge, but none of them needed another intervention.
Figure 2. The outcome of the empyema patients subjected to the SAFE approach based on the underlying diagnosis. SAFE: Start Away From Empyema.
The median (IQR) duration of hospital stay among studied patients was 5 (2), ranging from three to eight days. It was observed that eight patients (32%) developed fever post VAST procedure. The pain was reported in three patients (12%), and prolonged air leak was reported in three patients (12%), while minor bleeding occurred in four patients (16%). Forty percent had no complications.
DISCUSSION
Uniportal VATS approach was initiated as a minimally invasive technique for minor operations via Migliore et al.[7,8] starting in 1998 in Italy then by Rocco et al.[9], mainly for wedge resection in 2004. However, its tremendous popularity was derived by anatomical resection since 2011[10] and later by extended resections and awake non intubated surgery[11,12]. Uniportal VATS decortication was not meet the same acceptance as debridement, evacuation of retained hemothorax, thymectomy, and other non-resection cases. This might be due to the nature of the pathology as the inflammatory condition with dense adhesions narrows space to work. Moreover, one of the crucial points of uniportal VATS is the appropriate length between the entry site and targeted areas. Hence, it is necessary to plan precisely to avoid the area of interest when making the port incision so that all the surgical instruments have a comfortable working angle, which is usually challenging to achieve in late-stage empyema with narrow crowded intercostal space. This difficulty was reflected on less favor of uniportal VATS in those patients, heterogeneity of surgical steps, the extent of the operation, exact definition, publications on the learning curve, and how to do it[3].
We enrolled 25 patients in this study with a mean age of 38.24 years and aged 22-63 years. This age range is unlike other similar studies investigating uniportal VATS decortication, where their mean age was 60.0 ± 15.2 and 55 ± 16[2,5]. This might reflect the magnitude of infectious disease among the younger population without significant comorbidities in developing countries and explain the long duration of symptoms before the intervention. They could tolerate this wait time, as the mean duration was 25.6 days among patients with successful outcomes. In comparison, it was 43.6 days among patients with partial success, unlike Bongiolatti et al.[2], where they had only 19 ± 9 days. EACTS expert consensus statement for surgical management of pleural empyema[13] showed that patients with symptoms of more than five weeks should go for open surgery from the beginning. This might also contribute to partial success in those cases.
The underlying diagnosis was bacterial empyema thoracis (60%), tuberculous effusion (28%), and malignant effusion (12%). Most patients (88%) had successful outcomes while (12%) had partially successful outcomes. Even though the duration of illness was significantly longer among patients with partial success, it was noticed that all cases with partial success were infected malignant effusion (they had infection over malignant effusion not infection with/by malignant effusion). There was a statistically significant relationship between the underlying diagnosis and the success rate of VATS. Different outcomes among the study group had insignificant differences regarding chest X-ray and chested US findings. We reported complete success in all empyema and tuberculous effusion cases, while none of the malignant cases achieved complete resolution. This is consistent with the recent ERS/EACTS statement on managing malignant pleural effusions. Where VATS pleurectomy was associated with complications, and more extended hospital stays, with no additional benefit in terms of pleurodesis success[14].
We could not conclude that previous intervention increases the difficulty of decortication as all our patients had at least one intervention before. This point was not reported in most previous trials, unlike other risk factors such as smoking, diabetes, and renal insufficiency. The mean duration of hospital stay among all patients with different outcomes was 5.84 days. This was much lower than other studies[2,5,15], partially attributed to the younger age group in the current study with fewer comorbidities. Another explanation was our service protocol of discharging patients following chest tube removal[16]. The difference in-hospital stay of VATS decortication was emphasized by van Middendorp et al.[5] Some hospitals did not discharge patients home until they were fit to go. In contrast, others transferred patients to pulmonary service to get rehabilitation. Therefore, patients were discharged much early[5], while other studies demonstrated much less hospital stay as they discharged patients home with two chest tubes[15].
There was no mortality or significant complication in our groups. The complications were minor; fever in 8 cases (32%), pain in 3 cases (12%), and bleeding in 4 cases (16%), while no complications were reported in 10 cases (40%). Nevertheless, all patients get only one chest tube, and we used an ordinary chest tube system with no negative or electronic portable suction device.
Most previous studies provided a minor operative description of VATS decortication regarding the surgical steps. Moreover, they included VATS debridement, de-loculation, and decortication in the same group, mainly due to a small number of cases[2,4,5,17]. This, in turn, affected the overall outcome and made comparison difficult. More attention to putting standard steps for each operation and unifying definitions were essential as in van Middendorp et al.[5], who referred to uniportal VATS as (uVATS) while multiport VATS as complete VATS (cVATS). This might confuse readers that uniportal VATS was incomplete or not so good. Zhou et al.[15] described the need to remove a segment from the rib to overcome the problem of crowded ribs, but they called the approach uniportal VATS decortication as they did not use a metal rib spreader. They also argued that they removed all parietal and visceral peels, unlike other studies[3,17], they claim that this restore the deformed thorax to normal more quickly. Bongiolatti et al.[2] used the chest ultrasound to locate the empyema pouch intraoperatively; then, they tailored the single port at the most dependent point of the pouch. Unlike Bongiolatti’s technique, we tried to start away from the empyema pouch as previously described, but we did not tailor the incision each time based on imaging. We assumed that late-stage empyema was usually loculated posterior, and the site of the anterior axillary line at the fifth intercostal space would drive us away from the pouch. Our results were comparable to Bongiolatti et al.[2] in terms of no mortality, need for conversion, chest tube duration, and need for another intervention.
In conclusion, uniportal VATS decortication using the SAFE approach can be safe and effective for stage II and III empyema. More standard operative steps and definitions for VATS decortication should be developed to expand the approach and help to shorten the learning curve.
DECLARATIONS
AcknowledgmentAuthors would like to thank Prof. Hany Hasan Elsayed of Ain Shams University, Cairo, Egypt. for his fruitful suggestion naming the approach; SAFE approach. authors also like to thank Dr. Mariam Elkhayat of Assiut University, Egypt for her help in statistical analysis section of this research.
Authors’ contributionsMade substantial contributions to conception and design of the study and performed data analysis and interpretation: Elkhayat H, Gamal M, Ahmed Y
Performed data acquisition, as well as provided administrative, technical, and material support: Aboelfadel A, Omer A
Availability of data and materialsData can be provided as a Supplementary File in the journal if needed.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateThis work was performed in Cardiothoracic Surgery operative room. Institutional ethical committee of Assiut university faculty of medicine, Assiut, Egypt approve the study and clinical trial registration number was obtained (ClinicalTrials.gov Identifier: NCT03172052) with informed consent obtained from the patient for enrollment in the study.
Consent for publicationConsent for intervention and consent for publication were obtained from every patient as requested by our institutional ethical committee.
Copyright© The Author(s) 2022.
Supplementary MaterialsREFERENCES
1. Bobbio A, Bouam S, Frenkiel J, et al. Epidemiology and prognostic factors of pleural empyema. Thorax 2021;76:1117-23.
2. Bongiolatti S, Voltolini L, Borgianni S, et al. Uniportal thoracoscopic decortication for pleural empyema and the role of ultrasonographic preoperative staging. Interact Cardiovasc Thorac Surg 2017;24:560-6.
3. Elkhayat H. Uniportal VATS approach for treatment of empyema: Challenges and recommendations. Multimed Man Cardiothorac Surg 2018:2018.
4. Elkhayat H, Sallam M, Kamal M, Abdalla EM. Thoracoscopic decortication for stage III empyema; a minimal invasive approach in a delayed presentation disease. Journal of the Egyptian Society of Cardio-Thoracic Surgery 2018;26:301-7.
5. van Middendorp LB, Franssen S, Gillissen S, et al. Uniportal video-assisted thoracoscopy is a safe approach in patients with empyema requiring surgery. J Thorac Dis 2020;12:1460-6.
6. Yang PC, Luh KT, Chang DB, Wu HD, Yu CJ, Kuo SH. Value of sonography in determining the nature of pleural effusion: analysis of 320 cases. AJR Am J Roentgenol 1992;159:29-33.
7. Migliore M, Deodato G. A single-trocar technique for minimally-invasive surgery of the chest. Surg Endosc 2001;15:899-901.
8. Migliore M. Efficacy and safety of single-trocar technique for minimally invasive surgery of the chest in the treatment of noncomplex pleural disease. The Journal of Thoracic and Cardiovascular Surgery 2003;126:1618-23.
9. Rocco G, Martin-ucar A, Passera E. Uniportal VATS wedge pulmonary resections. The Annals of Thoracic Surgery 2004;77:726-8.
10. Gonzalez D, Paradela M, Garcia J, Dela Torre M. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5.
11. Lyscov A, Obukhova T, Ryabova V, Sekhniaidze D, Zuiev V, Gonzalez-Rivas D. Double-sleeve and carinal resections using the uniportal VATS technique: a single centre experience. J Thorac Dis 2016;8:S235-41.
12. Elkhayat H, Gonzalez-Rivas D. Non-intubated uniportal video-assisted thoracoscopic surgery. J Thorac Dis 2019;11:S220-2.
13. Scarci M, Abah U, Solli P, et al. EACTS expert consensus statement for surgical management of pleural empyema. Eur J Cardiothorac Surg 2015;48:642-53.
14. Bibby AC, Dorn P, Psallidas I, et al. ERS/EACTS statement on the management of malignant pleural effusions. Eur Respir J 2018;52:1800349.
15. Zhou Y, Li X, Dai J, et al. Uniportal Thoracoscopic Decortication for stage III tuberculous empyema with severe rib crowding. Ann Thorac Surg 2021;112:289-94.
16. Nafady, Magda Ahmed Mohammed, Sahra Zaki Azer, Hussein El Khayat. Effect of educational nursing protocol on minimizing patients’ complications after thoracoscopic surgery. Assiut Scientific Nursing Journal 2019;7:69-77.
Cite This Article
How to Cite
Elkhayat H, Gamal M, Ahmed Y, Aboelfadel A, Omer A. Uniportal thoracoscopic decortication: start away from empyema approach. Mini-invasive Surg. 2022;6:27. http://dx.doi.org/10.20517/2574-1225.2022.11
Download Citation
Export Citation File:
Type of Import
Tips on Downloading Citation
Citation Manager File Format
Type of Import
Direct Import: When the Direct Import option is selected (the default state), a dialogue box will give you the option to Save or Open the downloaded citation data. Choosing Open will either launch your citation manager or give you a choice of applications with which to use the metadata. The Save option saves the file locally for later use.
Indirect Import: When the Indirect Import option is selected, the metadata is displayed and may be copied and pasted as needed.
























Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.