Analysis of measures against mechanical complications in circumferential minimally invasive surgery for adult spinal deformity
Abstract
Aim: We evaluated the reduction of mechanical complications (MCs) in circumferential minimally invasive spinal surgery (c-MIS) to treat adult spinal deformity (ASD) using lateral lumbar interbody fusion and a percutaneous pedicle screw.
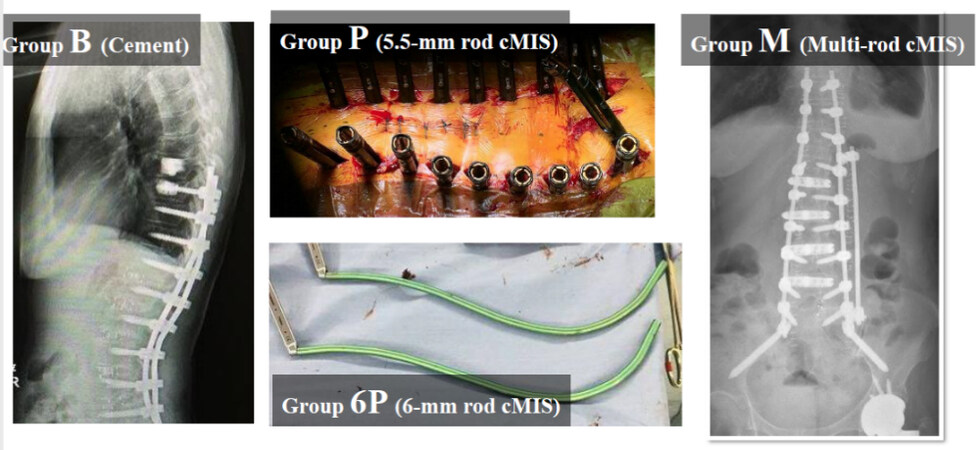
Methods: Patients with ASD who underwent c-MIS with a follow-up period of > 24 months were enrolled. Groups were as follows: c-MIS using 5.5 mm rods (P group), c-MIS using a 5.5 mm single rod with cement augmentations in the upper instrumented vertebra (UIV)/UIV + 1 (B group), c-MIS using 6 mm rods (6P group), and multi-rod
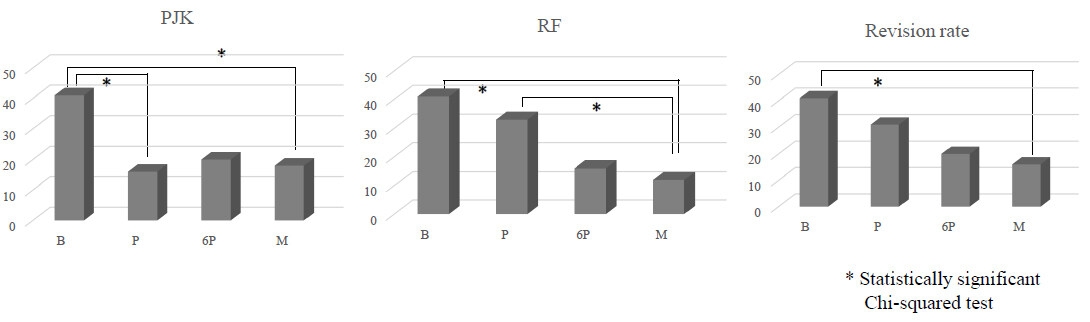
Results: Overall, 146 patients with ASD who underwent c-MIS were included. The incidence of PJK was significantly lower in the P and M groups than in the B group, and rod fracture was significantly lower in the M group than in the B and P groups. In the MC group, preoperative PT, postoperative PI-LL, and PSA were significantly larger than those in the non-MC group. Use of the 5.5 mm single rod and postoperative PI-LL were significant risk factors for MCs.
Conclusion: The complication incidence decreased with improvements in surgical techniques and measures. Use of the 5.5 mm single rod and postoperative PI-LL were significant risk factors for MCs.
Keywords
INTRODUCTION
The prevalence of adult spinal deformity (ASD) is increasing as the relative population of older individuals increases and corrective surgery becomes widespread. While surgical treatment significantly benefits patients with ASD[1,2], the incidence of complications from ASD surgery reportedly ranges from approximately 8.4%-68%, which is 4-8 times that of idiopathic scoliosis. The invasiveness of the surgery is a further concern[3,4].
In 2006, Ozgur et al. reported a novel approach to extreme lateral interbody fusion (XLIF®, Nuvasive Inc., San Diego, CA, USA), which enabled minimally invasive interbody release and interbody fusion[5]. In addition, circumferential minimally invasive surgery (c-MIS) with percutaneous pedicle screw (PPS) and lateral lumbar interbody fusion (LLIF) for ASD is gaining popularity[6,7]. However, various complications, such as proximal junctional kyphosis (PJK)/proximal junctional failure (PJF)[8,9], rod fracture (RF)[10-12], and coronal imbalance (CI)[13,14], still occur at a consistent rate; therefore, countermeasures are important.
METHODS
Patient selection
This study was approved by the institutional review board of the Kansai Medical University Hospital (Approval No. 2020189) and was conducted after obtaining informed consent from all patients involved. Written informed consent was also obtained from the patients for the publication of this report and any accompanying images. The inclusion criteria were as follows: age > 45 years, sagittal vertical axis (SVA)
Radiological evaluation
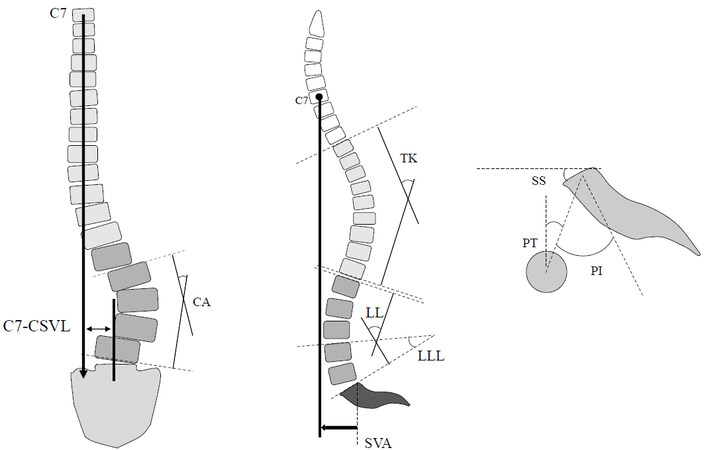
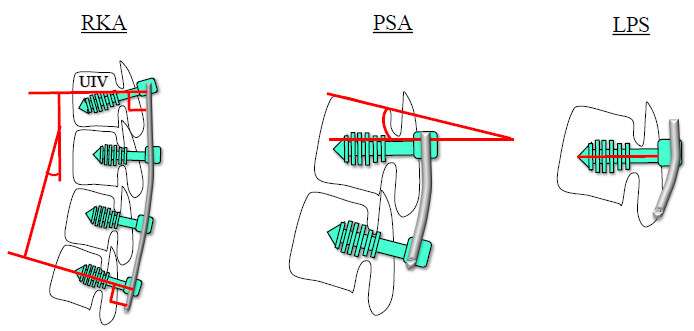
Standing posteroanterior and lateral whole-spine radiographs were recorded at preoperative baseline and final follow-up. The following spinopelvic parameters were investigated using the current standard method: PI, LL, lower LL (LLL), PT, thoracic kyphosis, and SVA [Figure 2]. The following implant-related parameters were also investigated with reference to the report by Ishihara et al.[16]: the kyphotic angle of the rod in the UIV-L1 rod kyphotic angle (RKA), the angle between the pedicle screw (PS) and cranial endplate in the UIV [pedicle screw angle (PSA)], and the length of PS in the UIV [length of PS (LPS); Figure 3]. PJK was defined as the postoperative proximal junctional angle (PJA) between the caudal endplate of the UIV and the cephalad endplate of the UIV + 2 ≥ 10° and at least 10° greater than the preoperative measurements[17].
Figure 2. Spinopelvic parameters. LL: Lumbar lordosis; LLL: lower LL; TK: thoracic kyphosis; SS: sacral slope; PT: pelvic tilt; PI: pelvic incidence; SVA: sagittal vertical axis; CSVL: central sacrum vertical line; CA: cobb angle.
Statistical analysis
Radiographic and clinical parameters were analyzed using the Mann-Whitney U test or Wilcoxon signed-rank test for continuous data and the Chi-squared test for categorical data. Furthermore, logistic regression analysis was performed based on the results of the univariate analysis. Statistical significance was set at
RESULTS
Demographics
Based on the selection criteria, 156 patients were initially included in the study. As 10 patients were subsequently excluded (five underwent surgeries from the upper thoracic vertebrae to the ilium and five did not have sufficient radiological data), 146 patients were enrolled for the analysis. Demographic data are shown in Table 1. The mean age at surgery was 73.3 years (range, 48-83 years), and the mean follow-up period was 42.3 ± 18.2 months (range, 26-96 months). Female patients accounted for 75% of the study population (male:female = 1:3). No significant difference in age and sex was identified among the four groups; however, there was a significant difference in the follow-up period. Titanium alloy (TA) was used as the rod material only in the P, 6P, and M groups, whereas cobalt chromium (CCr) was used in more than half of the cases in the B group. The average bleeding volume was 732.0 ± 432.1 mL (anterior,
Demographic data
| B group | P group | 6P group | M group | Total | P-value | ||
| Cases | 17 | 51 | 45 | 33 | 146 | ||
| F/U (months) | 52.7 ± 3.8 | 45.4 ± 5.6 | 40.2 ± 1.8 | 34.3 ± 2.6 | 42.3 ± 18.2 | P < 0.001* | |
| Age (years) | 72.1 ± 4.4 | 72.8 ± 6.8 | 73.2 ± 7.1 | 72.0 ± 6.2 | 72.3 ± 6.5 | n.s. | |
| Sex (male:female) | 5:12 | 12:39 | 12:33 | 8:25 | 36:108 | n.s. | |
| Rod material (CCr:TA) | 17:0 | 0:51 | 0:45 | 0:33 | 15:131 | **(B vs. P, 6P, M) | |
| Operative time | Ant (min) | 156.6 ± 40.9 | 133.3 ± 31.5 | 115.7 ± 26.6 | 103.7 ± 25.3 | 130.7 ± 45.9 | *(6P vs. M) *(B vs. P) **(B,P vs. M) |
| Post (min) | 318.8 ± 48.1 | 261.3 ± 39.4 | 222.3 ± 26.6 | 202.5 ± 42.9 | 242.7 ± 76.5 | *(P vs. M) **(B vs. P, 6P, M) | |
| Total (min) | 475.4 ± 65.0 | 392.7 ± 52.6 | 354.1 ± 37.1 | 315.2 ± 132.1 | 365.7 ± 158.2 | *(6P, P vs. M) **(B vs. P, 6P, M) | |
| Blood loss | Ant (mL) | 145.8 ± 166.6 | 115.8 ± 167.6 | 128.4 ± 148.8 | 124.1 ± 77.6 | 129.1 ± 155.0 | n.s. |
| Post (mL) | 912.8 ± 544.6 | 650.3 ± 309.4 | 506.6 ± 218.4 | 412.1 ± 296.2 | 603.2 ± 309.2 | *(B vs. P) **(B vs. 6P, M) | |
| Total (mL) | 1058.7 ± 6.8.6 | 760.1 ± 372.1 | 635.1 ± 320.8 | 437.3 ± 289.4 | 732.0 ± 432.1 | *(P vs. M, B) **(B vs. 6P, M) | |
Radiographic parameters
Spinopelvic parameters
The spinopelvic parameters revealed no statistically significant differences between the four groups [Table 2].
Spinopelvic parameters and implant-related parameters
| B group (n = 17) | P group (n = 51) | 6P group (n = 45) | M group (n = 33) | P-value | |
| Preop. PI (°) | 43.5 ± 13.1 | 46.1 ± 11.7 | 43.3 ± 12.1 | 46.5 ± 11.1 | n.s. |
| Postop. PI (°) | 43.8 ± 12.7 | 47.0 ± 10.9 | 44.5 ± 11.9 | 45.2 ± 12.1 | n.s. |
| Preop. LL (°) | 7.2 ± 13.5 | 6.2 ± 12.1 | 7.2 ± 12.8 | 4.0 ± 13.1 | n.s. |
| Postop. LL (°) | 46.2 ± 9.8 | 48.8 ± 10.2 | 46.2 ± 11.1 | 48.8 ± 10.2 | n.s. |
| Preop. PI-LL (°) | 33.9 ± 12.5 | 38.5 ± 15.3 | 36.9 ± 14.8 | 42.5 ± 15.4 | n.s. |
| Postop. PI-LL (°) | 1.2 ± 14.3 | 2.6 ± 13.4 | 1.2 ± 12.3 | 2.6 ± 11.2 | n.s. |
| Preop. PT (°) | 29.5 ± 7.2 | 30.7 ± 6.8 | 29.5 ± 8.5 | 30.7 ± 7.5 | n.s. |
| Postop. PT (°) | 18.9 ± 6.2 | 20.9 ± 6.9 | 20.2 ± 7.1 | 18.9 ± 6.8 | n.s. |
| Preop. TK (°) | 21.3 ± 8.7 | 16.2 ± 9.4 | 22.5 ± 9.9 | 16.2 ± 7.2 | n.s. |
| Postop. TK (°) | 38.8 ± 9.3 | 37.7 ± 10.1 | 39.8 ± 8.3 | 36.7 ± 7.5 | n.s. |
| RKA (°) | 10.5 ± 7.2 | 18.9 ± 8.9 | 19.2 ± 9.3 | 18.7 ± 9.2 | P < 0.001*** |
| PSA (°) | 2.5 ± 5.2 | 4.1 ± 3.8 | 18.1 ± 5.6 | 19.3 ± 6.2 | P < 0.001** |
| LPS (mm) | 36.4 ± 2.3 | 35.7 ± 2.4 | 42.5 ± 2.7 | 43.1 ± 2.6 | P < 0.001** |
Implant-related parameters
RKA in the P, 6P, and M groups was significantly larger than that in the B group (P < 0.001). PSA and LPS in the 6P and M groups were significantly larger than those in the other groups (P < 0.001; Table 2).
Complications
The incidence of PJK decreased in the P, 6P, and M groups, and the incidence of PJK in the P and M groups was significantly lower than that in the B group [P = 0.029 (B vs. M) and 0.017 (B vs. P)]. The incidence of RF in the M group was significantly lower than that in the B and P groups [P = 0.004 (B vs. M) and 0.013
Figure 4. Complications: B group: Balloon kyphoplasty in the upper instrumented vertebra (UIV)/UIV + 1 to prevent proximal junctional kyphosis; P group: circumferential minimally invasive surgery (c-MIS) using 5.5 mm rods; 6P group: c-MIS using 6 mm rods; M group: multi-rod c-MIS. PJK: Proximal junctional kyphosis; RF: rod fracture.
Complications
| B group (n = 17) | P group (n = 51) | 6P group (n = 45) | M group (n = 33) | Total (n = 146) | P-value | |
| PJK/PJF | 8 (47.1%) | 8 (16.6%) | 9 (20.9%) | 9 (18.7%) | 33 (22.6%) | *(B vs. P, M) |
| RF | 11 (64.7%) | 16 (33.3%) | 7 (16%) | 6 (12.5%) | 40 (27.8%) | *(B, P vs. M) |
| Union failure | 9 (52.0%) | 14 (33.3%) | 7 (16%) | 6 (12.5%) | 36 (26.5%) | *(B, P vs. M) |
| Total revision rate | 11 (64.7%) | 15 (31.2%) | 9 (20.9%) | 8 (16.6%) | 43 (29.9%) | *(B, vs. M) |
| PJK/PJF | 7 (41.2%) | 6 (12.5%) | 6 (13.9%) | 3 (6.2%) | 22 (15.0%) | *(B vs. P, M, 6P) |
| RF | 10 (58.8%) | 12 (25.0%) | 5 (11.6%) | 4 (8.3%) | 31 (21.0%) | * (B vs. 6P, M) |
Risk factors for MCs
In the MC group, 5.5 mm single rods were used more frequently than 6 mm single rods and 5.5 mm multi-rods, and CCr rods were used more often than TA rods [Table 4]. Among the various parameters, those in the MC group were significantly larger in terms of preoperative PT, postoperative PI-LL, and PSA [Table 5] compared with the non-MC group. Logistic regression analysis identified the use of a single 5.5 mm rod and postoperative PI-LL as significant risk factors for MCs. Receiver operating characteristic analysis of MCs using postoperative PI-LL revealed a cutoff value of 7° [area under the curve (AUC), 0.599].
Demographic data (MC group vs. non-MC group)
| Whole Group (n = 146) | Group non-MCs (n = 85) | Group MCs (n = 61) | ||
| Age (years) | 72.3 ± 6.5 (48-83) | 72.1 ± 6.9 | 73.2 ± 7.7 | |
| Rate of women (%) | 77.3 | 80.1 | 77.1 | |
| Period of follow-up (months) | 42.3 ± 18.2 (26-69) | 40.7 ± 6.3 | 40.6 ± 6.2 | |
| Rod diameter/ number in construct | 5.5 mm/2 rods | 66(45%) | 30 | 36* |
| 6 mm/2 rods | 45(31%) | 31 | 14 | |
| 5.5 mm/3 rods | 35 (24%) | 24 | 11 | |
| Rod material | CCr | 17 | 3 | 14** |
| TA | 131 | 83 | 48 | |
| Number of levels fused | 10.3 ± 0.5 (10-13) | 10.3 ± 0.5 | 10.4 ± 05 | |
| Cement augmentation in UIV/UIV+1 | 17 | 3 | 14** | |
| Number of LLIF | 4.0 ± 0.5 (3-6) | 4.0 ± 03 | 4.1 ± 05 | |
| UIV (case) | T8 | 3 (2%) | 2 | 1 |
| T9 | 39 (27%) | 20 | 19 | |
| T10 | 104 (71%) | 63 | 41 | |
Spinopelvic parameters and implant-related parameters (MC group vs. non-MC group)
| Group MCs (n = 85) | Group non-MCs (n = 61) | P-value | |
| Pre-PI (°) | 48.8 ± 11.6 | 46.7 ± 11.6 | 0.185 |
| Post-PI (°) | 50.0 ± 10.7 | 47.2 ± 9.2 | 0.057 |
| Pre-LL (°) | 9.7 ± 16.5 | 7.2 ± 15.8 | 0.224 |
| LL after LLIF (°) | 32.6 ± 10.7 | 31.8 ± 10.9 | 0.489 |
| Post-LL (°) | 44.8 ± 9.8 | 46.8 ± 10.6 | 0.409 |
| Pre-PI-LL (°) | 38.1 ± 18.8 | 39.6 ± 15.0 | 0.520 |
| Post-PI-LL (°) | 4.0 ± 11.4 | 0 ± 10.2 | *0.035 |
| Pre-PT (°) | 32.2 ± 11.54 | 30.6 ± 10.2 | 0.480 |
| Post-PT (°) | 18.9 ± 9.7 | 16.1 ± 8.6 | *0.049 |
| Pre-TK (°) | 21.6 ± 14.2 | 20.8 ± 8.6 | 0.895 |
| Post-TK (°) | 37.4 ± 10.1 | 37.9 ± 10.6 | 0.724 |
| Pre-LLL (°) | 20.4 ± 12.5 | 24.0 ± 9.8 | 0.092 |
| Post-LLL (°) | 30.4 ± 8.7 | 30.8 ± 7.3 | 0.991 |
| RKA (°) | 18.8 ± 6.9 | 20.1 ± 6.0 | 0.101 |
| PSA (°) | 6.4 ± 8.2 | 8.9 ± 6.8 | *0.019 |
| LPS (mm) | 19.3 ± 6.0 | 22.0 ± 4.3 | *0.037 |
DISCUSSION
Global alignment and mechanical complications
Yilgor et al. reported the importance of global alignment and proportion in the prevention of MCs[15]. Pizones et al. and Sebaaly et al. reported that restoring the ideal Roussouly sagittal alignment in ASD surgery decreases the risk of mechanical complications[18,19]. All these reports combine PJK and RF under the definition of MCs and describe the importance of global spinal proportions in the prevention of MCs. However, Kwan et al. reported that spinal alignment based on the global alignment and proportion score is not associated with an increased risk of MCs[20]. We previously reported risk factors for PJK[16]. In that study, we reported that the occurrence of PJK was not associated with inflection point height and restoration to alignment based on the Roussouly classification. In the present study, postoperative PI-LL was a risk factor for MCs with a cutoff value of 7°. This result indicates that sufficient alignment correction is important in the prevention of MCs. Conversely, there was no significant difference in LLL between the two groups, and the spinal proportions between the two groups were similar. From the above results, we can speculate that insufficient alignment correction is more strongly related to MCs than to spinal proportion. We considered that the results may be expected to differ between the study in which PJK and RF were collectively analyzed as MCs and the study in which PJK and RF were analyzed separately. We further consider that PJK and RF occur for different reasons and that grouping both of them under the label of mechanical complications is a reason for the confusion in investigating the causes of each. Therefore, the causes of PJK and RF should be investigated separately.
PJK/PJF
Although PJK is asymptomatic in most cases, it sometimes presents with serious symptoms such as pain and paralysis[21]. PJK is believed to be caused by multiple factors including age, preoperative SVA, thoracolumbar spinal muscle mass, overcorrection, the level of the UIV, the type of anchored instrumentation for UIV fixation, soft tissue damage around the UIV, fixation to the pelvis, UIV tilt angle, and terminal rod contour[8,16,21-26]. Of these factors, we consider the terminal rod contour to be the most important. We previously reported that inadequate kyphosis of the terminal rod and overcorrection were risk factors for PJK[16]. To reduce PJK after c-MIS for the treatment of ASD using LLIF and PPS, we have also been undertaking the following four measures: (1) inserting a pedicle screw at the thoracic level using the PPS technique to preserve the posterior soft tissues such as the paraspinal muscle, facet joint capsule, supraspinous ligament, and interspinous ligament; (2) inserting longer pedicle screws in the caudal direction obliquely at the UIV to prevent PS back-out; (3) ensuring sufficient kyphosis of the terminal rod contour for postoperative reciprocal change[16]; and (4) targeting postoperative LL with satisfactory PI-10 < LL < PI to avoid overcorrection[16]. In the present study, the incidence rate of PJK was higher in group B than in the other groups. There are two reasons for this. The first is the high rigidity of the CCr rods. CCr rods were used in all cases in Group B. Han et al. reported that PJK occurs more frequently in patients with CCr rods than in those with TA rods[27]. They considered that when a more rigid CCr rod is used, the increased stiffness of the vertebral body at the proximal end of fixation and the consequent load on the adjacent disc becomes a factor in PJK. Lange et al. and Cammarata et al. reported that a more gradual transition from instrumented to non-instrumented vertebra is important[28,29], and that the use of transition rods is desirable. In this study, it is speculated that the incidence rate of PJK was higher in group B than in the other groups due to excessive stress applied between adjacent vertebrae due to more rigid fixation using CCr rods with cement augmentation.
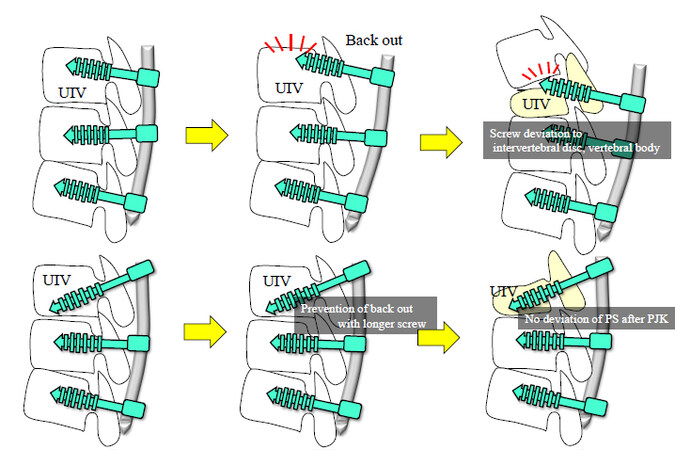
In addition, Bess et al., in their study on finite element analysis, reported that the use of a posterior tether rather than PS and hook is useful for the prevention of PJK[30]. The second reason for the higher PJK incidence is that RKA, PSA, and LPS were smaller in group B than in the other groups. We focused on kyphosis of the terminal rod to make the rod suitable for postoperative reciprocal change in the thoracic spine. Thoracic kyphosis, which had been compensated for preoperatively due to a decrease in LL, increased due to reciprocal changes after corrective surgery[16]. We speculate that kyphosis of the terminal rod was one of the reasons for the decreased PJK that made the rod suitable for postoperative reciprocal change of the thoracic spine. Insufficient RKA, as we reported in the past, is a cause of PJK because it is not compatible with postoperative reciprocal change. Increasing the PSA increases the strength of the pull-out of the screw and also prevents screw deviation to the cranial disc and cranial vertebral body when PJK occurs. Further, it is important to insert a longer PPS in the caudal direction rather than parallel to the endplate. The purpose of this is to increase pull-out strength and prevent screw penetration into the cranial disc and cranial vertebral body after a UIV fracture [Figure 5]. Oe et al. reported that longer screws can reduce the stress on the UIV and UIV fractures[31]. There are also some reports that the reduction of posterior soft tissue damage using PPS is useful in the prevention of PJK[22,32]. In all groups, posterior surgery was performed with PPS. However, RKA and PSA were significantly lower and LPS was significantly shorter in the B group than in the other groups. Therefore, in the present study, it is difficult to conclude whether preservation of the posterior soft tissue by using PPS is the primary factor that affects the prevention of PJK. It is speculated that these measures contributed to the prevention of PJF and its associated complications, such as PS back-out and secondary fractures of UIV + 1.
Figure 5. Inserting longer screws in the caudal direction obliquely at the UIV. UIV: Upper instrumented vertebra; PJK: proximal junctional kyphosis.
Theologis et al. and Martin et al. reported the usefulness of cement augmentation in PJK prevention[33,34]. In the B group in the present study, cement augmentation was performed in the UIV and UIV + 1 to prevent PJK. However, the incidence of PJK was 41.3%, which was higher than that in the other groups. Increasing the bone strength of the vertebral body with cement augmentation to prevent screw back-out and vertebral body fracture did not prevent PJK. Conversely, the RKA, PSA, and LPS in the B group were significantly smaller than those in the other groups. Furthermore, the PSA and LPS in the B groups were significantly smaller than those in the 6P and M groups. From the above results, we could expect that the terminal rod contour, PSA, and PSL are more important factors for determining the prevention of PJK than the increase in bone strength and rigidity of instrumentation.
The inflection point (IP) was also very important. According to Roussouly et al., the spinal alignment of healthy people can be classified into four types, and the IP moves toward the cranial side as the PI increases[35]. Jakinapally et al. reported that the incidence of PJK in patients with inflection vertebra at T12 or cranially was significantly higher (69%) than that at L1 or caudally (26%)[36]. We reported that RKA in the UIV to L1 requires 13.5° or more to prevent PJK[16]. Based on the report by Roussouly et al.[35], we speculate that we should create a rod contour with the IP moved further cranially if the patient's PI is high and with the IP moved more caudally if the patient’s PI is low. Considering the findings of our previous report and Jakinapally et al.’s report[36], we need to create a rod contour with a thoracic kyphosis ≥ 13° and an IP of L1 or lower.
There are also some reports that suggest that overcorrection is a risk factor for PJK[16,27,37]. Mechanistically, this is expected to correct the global balance by developing PJK when overcorrection results in a negative SVA[16]. We consider that PI-10 < LL < PI is appropriate for the correction goal in ASD surgery[16].
RF
RF is a frequent implant-related complication following ASD surgery. Previous studies have shown a high incidence (range 6.8%-22%) of RF following corrective fusion surgery in patients treated for ASD[10,11,38,39]. Several risk factors have been reported for the development of RF, such as older age, higher BMI, history of previous spine surgery, performance of a pedicle subtraction osteotomy, use of CCr rods, greater baseline sagittal spinopelvic malalignment (SVA, PT, and PI-LL mismatch), and greater magnitude of sagittal spinopelvic malalignment correction with surgery (SVA and PI-LL mismatch)[10,11,39]. In c-MIS for the treatment of ASD, there is a significant risk that if the bone surface for grafting is narrow, bone grafting other than interbody fusion cannot be performed. Accordingly, the pseudarthrosis rate is higher than that of conventional open surgery[40]. Moreover, since the bone surface area available for bone fusion is narrow in c-MIS, bone fusion takes longer. RF in c-MIS develops because the durability of the rod decreases before bone fusion is achieved. Therefore, it is important to increase rod durability by using additional rods to prevent the breakage that may occur before bone fusion to increase the bone fusion rate. Increasing the durability of the rod will promote spontaneous bone fusion of facet joint and intervertebral bridging[41]. Previous reports have shown that multiple rods reduce RF after ASD, and the benefit of multiple rods is gradually being recognized[42-44]. In the present study, the incidence of RF tended to decrease in the 6P group and significantly decreased in the M group, confirming the benefit of multiple rods for RF. Furthermore, in the logistic regression analysis in this study, the use of a 5.5 mm single rod and postoperative PI-LL were identified as significant risk factors for MCs. This result suggests that increasing the number of rods or rod diameter is more useful in the prevention of RF. Conversely, Pizones et al. and Sebaaly et al. reported that recovery to good alignment is important for the prevention of MCs[18,19]. In the present study, post PI-LL was detected as a risk factor for MCs, and the results were almost the same as in previous reports.
Surgical invasion/re-surgery rate
The amount of bleeding and the operation time peaked in group B and decreased with the improvement of the surgical procedure. The reason for this reduction in surgical invasion is due to the acquisition of surgical techniques and progression of the surgeon along the learning curve.
The re-surgery rate after open ASD surgery reportedly ranges from 9%-58%[9,45-49]. Hamilton et al. reported a 12% re-surgery rate after traditional open surgery; however, when less invasive procedures were employed, the rate increased to 27% in the HYB group but decreased to 11.1% in the c-MIS group[50]. In general, the re-surgery rate increases as follow-up durations increase, likely because failures such as RF, pseudoarthrosis, or adjacent segment disease may occur or become symptomatic several years after surgery. In the present study, the re-surgery rate was 41% in the B group; however, it was 20% in the 6P group and 16% in the M group, which is a significant decrease. The reason for this is that, although there are differences in the follow-up period, the above-mentioned measures against various complications were effective. However, further long-term follow-up is required in this regard.
Limitations
This study has four limitations. First, this was a retrospective, single-institution, historical study. In the future, a multi-center large-scale study would be desirable. Second, complications after surgery for ASD may have decreased as surgical techniques improved over time. The improvement of the surgical procedure produced a large bias in this study, and further detailed analysis using multivariate analysis or other methods is necessary in the future. Third, the effects of metal corrosion and corrosive products on tissues have not been investigated. Further investigation is needed in the future. Lastly, although bone mineral density (BMD) and its treatment may have significant impacts on PJK and RF, BMD was not evaluated in this study. Future studies should evaluate BMD in the context of osteoporosis treatment.
In conclusion, in the present study, we evaluated the effectiveness of measures against MCs from the clinical results of multiple surgical procedures to treat ASD, in addition to examining the risk factors for MCs. The incidence of MCs was highest in the B group and lowest in the M group. In the prevention of PJK, terminal rod contour, PSA, and LPS may be more important than tight fixation in the UIV. To reduce RF in c-MIS for ASD, it is necessary to obtain bone fusion before RF occurs, and it is important to increase the durability of the implant by using additional rods. The risk factors for MCs were the use of a single 5.5 mm rod and postoperative PI-LL.
DECLARATIONS
Authors’ contributionsMade substantial contributions to conception and design: Ishihara M
Performed data acquisition: Ishihara M
Investigation: Ishihara M, Adachi T, Tani Y, Paku M, Tanaka T, Masada K
Analyzed and interpreted the data: Ishihara M, Taniguchi S
Review and Editing: Taniguchi S, Kotani Y, Saito T
Supervision and Project Administration: Saito T
Supervised the study: Ishihara M
All authors approved the manuscript for publication.
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateThis study was approved by the institutional review board of the Kansai Medical University Hospital (approval no.: 2020189) and was conducted after obtaining the consent of all patients.
Consent for publicationWritten informed consent was obtained from the patient for publication of this report and any accompanying images. A copy of the written consent form is available for review by the editor.
Copyright© The Author(s) 2022.
REFERENCES
1. Bridwell KH, Glassman S, Horton W, et al. Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study. Spine (Phila Pa 1976) 2009;34:2171-8.
2. Smith JS, Lafage V, Shaffrey CI, et al. International Spine Study Group. Outcomes of operative and nonoperative treatment for adult spinal deformity: a prospective, multicenter, propensity-matched cohort assessment with minimum 2-year follow-up. Neurosurgery 2016;78:851-61.
3. Smith JS, Klineberg E, Lafage V, et al. International Spine Study Group. Prospective multicenter assessment of perioperative and minimum 2-year postoperative complication rates associated with adult spinal deformity surgery. J Neurosurg Spine 2016;25:1-14.
4. Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG. The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976) 2007;32:2764-70.
5. Ozgur BM, Aryan HE, Pimenta L, Taylor WR. Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 2006;6:435-43.
6. Mummaneni PV, Park P, Fu KM, et al. Does minimally invasive percutaneous posterior instrumentation reduce risk of proximal junctional kyphosis in adult spinal deformity surgery? A propensity-matched cohort analysis. Neurosurgery 2016;78:101-8.
7. Haque RM, Mundis GM Jr, Ahmed Y, et al. International Spine Study Group. Comparison of radiographic results after minimally invasive, hybrid, and open surgery for adult spinal deformity: a multicenter study of 184 patients. Neurosurg Focus 2014;36:E13.
8. Maruo K, Ha Y, Inoue S, et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976) 2013;38:E1469-76.
9. Mok JM, Cloyd JM, Bradford DS, et al. Reoperation after primary fusion for adult spinal deformity: rate, reason, and timing. Spine (Phila Pa 1976) 2009;34:832-9.
10. Smith JS, Shaffrey CI, Ames CP, et al. International Spine Study Group. Assessment of symptomatic rod fracture after posterior instrumented fusion for adult spinal deformity. Neurosurgery 2012;71:862-7.
11. Smith JS, Shaffrey E, Klineberg E, et al. International Spine Study Group. Prospective multicenter assessment of risk factors for rod fracture following surgery for adult spinal deformity. J Neurosurg Spine 2014;21:994-1003.
12. Hamilton DK, Buza JA 3rd, Passias P, et al. International Spine Study Group. The fate of patients with adult spinal deformity incurring rod fracture after thoracolumbar fusion. World Neurosurg 2017;106:905-11.
13. Matsumura A, Namikawa T, Kato M, Hori Y, Hidaka N, Nakamura H. Factors related to postoperative coronal imbalance in adult lumbar scoliosis. J Neurosurg Spine 2020:1-7.
14. Lewis SJ, Keshen SG, Kato S, Dear TE, Gazendam AM. Risk factors for postoperative coronal balance in adult spinal deformity surgery. Global Spine J 2018;8:690-7.
15. Yilgor C, Sogunmez N, Boissiere L, et al. European Spine Study Group (ESSG). Global alignment and proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am 2017;99:1661-72.
16. Ishihara M, Taniguchi S, Adachi T, et al. Rod contour and overcorrection are risk factors of proximal junctional kyphosis after adult spinal deformity correction surgery. Eur Spine J 2021;30:1208-14.
17. Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C 2nd. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 2005;30:1643-9.
18. Pizones J, Moreno-Manzanaro L, Sánchez Pérez-Grueso FJ, et al. ESSG European Spine Study Group. Restoring the ideal Roussouly sagittal profile in adult scoliosis surgery decreases the risk of mechanical complications. Eur Spine J 2020;29:54-62.
19. Sebaaly A, Gehrchen M, Silvestre C, et al. Mechanical complications in adult spinal deformity and the effect of restoring the spinal shapes according to the Roussouly classification: a multicentric study. Eur Spine J 2020;29:904-13.
20. Kwan KYH, Lenke LG, Shaffrey CI, et al. AO Spine Knowledge Forum Deformity. Are higher global alignment and proportion scores associated with increased risks of mechanical complications after adult spinal deformity surgery? Clin Orthop Relat Res 2021;479:312-20.
21. Bridwell KH, Lenke LG, Cho SK, et al. Proximal junctional kyphosis in primary adult deformity surgery: evaluation of 20 degrees as a critical angle. Neurosurgery 2013;72:899-906.
22. Cahill PJ, Wang W, Asghar J, et al. The use of a transition rod may prevent proximal junctional kyphosis in the thoracic spine after scoliosis surgery: a finite element analysis. Spine (Phila Pa 1976) 2012;37:E687-95.
23. Hart RA, McCarthy I, Ames CP, Shaffrey CI, Hamilton DK, Hostin R. Proximal junctional kyphosis and proximal junctional failure. Neurosurg Clin N Am 2013;24:213-8.
24. Hart R, McCarthy I, Oʼbrien M, et al. International Spine Study Group. Identification of decision criteria for revision surgery among patients with proximal junctional failure after surgical treatment of spinal deformity. Spine (Phila Pa 1976) 2013;38:E1223-7.
25. Yagi M, Rahm M, Gaines R, et al. Complex Spine Study Group. Characterization and surgical outcomes of proximal junctional failure in surgically treated patients with adult spinal deformity. Spine (Phila Pa 1976) 2014;39:E607-14.
26. Yan P, Bao H, Qiu Y, et al. Mismatch between proximal rod contouring and proximal junctional angle: a predisposed risk factor for proximal junctional kyphosis in degenerative scoliosis. Spine (Phila Pa 1976) 2017;42:E280-7.
27. Han S, Hyun SJ, Kim KJ, Jahng TA, Kim HJ. Comparative study between cobalt chrome and titanium alloy rods for multilevel spinal fusion: proximal junctional kyphosis more frequently occurred in patients having cobalt chrome rods. World Neurosurg 2017;103:404-9.
28. Lange T, Schmoelz W, Gosheger G, et al. Is a gradual reduction of stiffness on top of posterior instrumentation possible with a suitable proximal implant? Spine J 2017;17:1148-55.
29. Cammarata M, Aubin CÉ, Wang X, Mac-Thiong JM. Biomechanical risk factors for proximal junctional kyphosis: a detailed numerical analysis of surgical instrumentation variables. Spine (Phila Pa 1976) 2014;39:E500-7.
30. Bess S, Harris JE, Turner AW, et al. The effect of posterior polyester tethers on the biomechanics of proximal junctional kyphosis: a finite element analysis. J Neurosurg Spine 2017;26:125-33.
31. Oe S, Narita K, Hasegawa K, et al. Longer screws can reduce the stress on the upper instrumented vertebra with long spinal fusion surgery: a finite element analysis study. Global Spine J 2021:21925682211018467.
32. Korkmaz M, Akgul T, Sariyilmaz K, Ozkunt O, Dikici F, Yazicioglu O. Effectiveness of posterior structures in the development of proximal junctional kyphosis following posterior instrumentation: A biomechanical study in a sheep spine model. Acta Orthop Traumatol Turc 2019;53:385-9.
33. Theologis AA, Burch S. Prevention of acute proximal junctional fractures after long thoracolumbar posterior fusions for adult spinal deformity using 2-level cement augmentation at the upper instrumented vertebra and the vertebra 1 level proximal to the upper instrumented vertebra. Spine (Phila Pa 1976) 2015;40:1516-26.
34. Martin CT, Skolasky RL, Mohamed AS, Kebaish KM. Preliminary results of the effect of prophylactic vertebroplasty on the incidence of proximal junctional complications after posterior spinal fusion to the low thoracic spine. Spine Deform 2013;1:132-8.
35. Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 2005;30:346-53.
36. Jakinapally S, Yamato Y, Hasegawa T, et al. Effect of sagittal shape on proximal junctional kyphosis following thoracopelvic corrective fusion for adult spinal deformity: postoperative inflection vertebra cranial to T12 is a significant risk factor. Spine Deform 2020;8:1313-23.
37. Lafage R, Schwab F, Glassman S, et al. International Spine Study Group. Age-Adjusted alignment goals have the potential to reduce PJK. Spine (Phila Pa 1976) 2017;42:1275-82.
38. Akazawa T, Kotani T, Sakuma T, Nemoto T, Minami S. Rod fracture after long construct fusion for spinal deformity: clinical and radiographic risk factors. J Orthop Sci 2013;18:926-31.
39. Barton C, Noshchenko A, Patel V, Cain C, Kleck C, Burger E. Risk factors for rod fracture after posterior correction of adult spinal deformity with osteotomy: a retrospective case-series. Scoliosis 2015;10:30.
40. Eastlack RK, Srinivas R, Mundis GM, et al. International Spine Study Group. Early and late reoperation rates with various MIS techniques for adult spinal deformity correction. Global Spine J 2019;9:41-7.
41. Ishihara M, Taniguchi S, Kawashima K, et al. Bone fusion morphology after circumferential minimally invasive spine surgery using lateral lumbar interbody fusion and percutaneous pedicle screws without bone grafting in the thoracic spine: a retrospective study. Medicina (Kaunas) 2022;58:496.
42. Hyun SJ, Lenke LG, Kim YC, Koester LA, Blanke KM. Comparison of standard 2-rod constructs to multiple-rod constructs for fixation across 3-column spinal osteotomies. Spine (Phila Pa 1976) 2014;39:1899-904.
43. Jung JM, Hyun SJ, Kim KJ, Jahng TA. Rod fracture after multiple-rod constructs for adult spinal deformity. J Neurosurg Spine 2019:1-8.
44. Ishihara M, Taniguchi S, Adachi T, et al. Conditions for achieving postoperative pelvic incidence-lumbar lordosis < 10° in circumferential minimally invasive surgery for adult spinal deformity. J Clin Med 2022;11:1586.
45. Pichelmann MA, Lenke LG, Bridwell KH, Good CR, O’Leary PT, Sides BA. Revision rates following primary adult spinal deformity surgery: six hundred forty-three consecutive patients followed-up to twenty-two years postoperative. Spine (Phila Pa 1976) 2010;35:219-26.
46. Sánchez-Mariscal F, Gomez-Rice A, Izquierdo E, Pizones J, Zúñiga L, Álvarez-González P. Survivorship analysis after primary fusion for adult scoliosis. Prognostic factors for reoperation. Spine J 2014;14:1629-34.
47. Charosky S, Guigui P, Blamoutier A, Roussouly P, Chopin D. Study Group on Scoliosis. Complications and risk factors of primary adult scoliosis surgery: a multicenter study of 306 patients. Spine (Phila Pa 1976) 2012;37:693-700.
48. Ha Y, Maruo K, Racine L, et al. Proximal junctional kyphosis and clinical outcomes in adult spinal deformity surgery with fusion from the thoracic spine to the sacrum: a comparison of proximal and distal upper instrumented vertebrae. J Neurosurg Spine 2013;19:360-9.
49. OʼShaughnessy BA, Bridwell KH, Lenke LG, et al. Does a long-fusion “T3-sacrum” portend a worse outcome than a short-fusion “T10-sacrum” in primary surgery for adult scoliosis? Spine (Phila Pa 1976) 2012;37:884-90.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Ishihara M, Taniguchi S, Adachi T, Tani Y, Paku M, Ando M, Kotani Y, Saito T. Analysis of measures against mechanical complications in circumferential minimally invasive surgery for adult spinal deformity. Mini-invasive Surg 2022;6:35. http://dx.doi.org/10.20517/2574-1225.2022.23
AMA Style
Ishihara M, Taniguchi S, Adachi T, Tani Y, Paku M, Ando M, Kotani Y, Saito T. Analysis of measures against mechanical complications in circumferential minimally invasive surgery for adult spinal deformity. Mini-invasive Surgery. 2022; 6: 35. http://dx.doi.org/10.20517/2574-1225.2022.23
Chicago/Turabian Style
Ishihara, Masayuki, Shinichirou Taniguchi, Takashi Adachi, Yoichi Tani, Masaaki Paku, Muneharu Ando, Yoshihisa Kotani, Takanori Saito. 2022. "Analysis of measures against mechanical complications in circumferential minimally invasive surgery for adult spinal deformity" Mini-invasive Surgery. 6: 35. http://dx.doi.org/10.20517/2574-1225.2022.23
ACS Style
Ishihara, M.; Taniguchi S.; Adachi T.; Tani Y.; Paku M.; Ando M.; Kotani Y.; Saito T. Analysis of measures against mechanical complications in circumferential minimally invasive surgery for adult spinal deformity. Mini-invasive. Surg. 2022, 6, 35. http://dx.doi.org/10.20517/2574-1225.2022.23
About This Article
Copyright
Data & Comments
Data

 Cite This Article 6 clicks
Cite This Article 6 clicks











Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.