Laparoscopic and robotic approaches for treatment of choledochal cysts in adults
Abstract
Background: While well-described for hepatic and pancreatic resection, the minimally invasive (MIS) approach in the treatment of choledochal cysts (CC) has been under-reported. Due to the technical complexity and steeper learning curve of minimally invasive biliary reconstruction, the MIS approach has not been as widely adopted in biliary surgery. We herein review the use of laparoscopic and robotic-assisted surgery in the treatment of CC.
Methods: A comprehensive review of the literature was performed on the use of laparoscopic and robotic-assisted surgery in the treatment of CC.
Results: Similar morbidity and mortality rates were noted among patients undergoing laparoscopic choledochal cyst resection (LCCR) compared with previous data from patients in the literature who had undergone an open approach (OCCR, open choledochal cyst resection); however, LCCR was associated with longer operative times and high conversion rates, largely attributable to the learning curve given the technically challenging nature of the procedure. The robotic platform (RCCR, robotic choledochal cyst resection) has been shown to offer an advantage in the hepaticojejunostomy anastomosis portion of CC resection vs. laparoscopy while providing comparable short-term outcomes compared with the LCCR approach.
Conclusion: A minimally invasive approach to CC likely has improved perioperative outcomes with shorter LOS, return to baseline function, as well as improved cosmesis vs. OCCR. Longer operative times with minimally invasive approaches to CC have been attributed to steep learning curves, which have improved over time as surgeons become more facile with this technique. Both LCCR and RCCR have demonstrated similar rates of long-term postoperative complications and overall survival when compared to OCCR.
Keywords
INTRODUCTION
Choledochal cysts (CC) are abnormal cystic dilations within the extrahepatic and intrahepatic biliary tree. CC are more common in East Asian populations and have a four-times higher incidence in female patients[1]. The most widely accepted classification system for CC was proposed in 1959 before being revised in 1977 to include intrahepatic cysts then further refined in 2003 to incorporate the presence of an abnormal pancreaticobiliary junction[2-4]. According to the Todani classification system[5], type I cysts are characterized by a cystic or fusiform dilation of the common bile duct (CBD) (IA involves the CBD and part or all of the common hepatic duct and extrahepatic portions of the left and right hepatic ducts, IB is a focal segmental dilation of the distal CBD, IC is a dilation of all the extrahepatic ducts, and ID is a cystic dilation of CBD and cystic duct), type II cysts are true diverticula of the extrahepatic bile ducts, type III cysts (i.e., choledochocele) are cystic dilations limited to the intraduodenal portion of the distal CBD that can be lined by either duodenal or biliary epithelium and are not associated with any malunion, type IV cysts are defined by the presence of multiple cysts and are divided into subtypes based on intrahepatic bile duct involvement (Type IV A - both intrahepatic and extrahepatic cystic dilations vs. Type IV B - only extrahepatic cysts); type V CC are defined by one or more cystic dilations of the intrahepatic ducts without extrahepatic involvement and is termed Caroli disease[6]. When Type V CC is associated with congenital hepatic fibrosis, it is termed Caroli syndrome and is typically inherited as an autosomal recessive trait[7]. In a subset of patients, CC can be associated with symptoms such as abdominal pain, nausea, vomiting, fever, and jaundice, consistent with cholangitis. Adult patients with CC may more commonly present with pancreatitis. Patients with type I, II, or IV cysts should typically undergo surgical resection due to the risk of malignancy, recurrent cholangitis, or recurrent pancreatitis. Patients with intrahepatic type IV cysts will often undergo a partial hepatectomy for the resection of the intrahepatic portion of the cyst which may be difficult to treat[8]. Among patients with CC, the incidence of malignancy approximates 10%[9]. In general, the preferred operative approach is surgical resection of the CC with a Roux-en-Y hepaticojejunostomy. A hepaticoduodenostomy is not typically performed in adults due to anatomic reasons as well as to avoid reflux into the biliary tree. Of note, patients with type III cysts require endoscopic treatment only if symptomatic. Patients with type V cysts generally receive supportive treatment unless the patient develops complications such as recurrent cholangitis or sepsis; treatment of type V cysts generally requires liver transplantation in the setting of progressive biliary cirrhosis and portal hypertension.
The application of minimally invasive surgery (MIS) has transformed various surgical subspecialties. Due to technological advancements, improved multidisciplinary planning, and advanced imaging techniques, MIS has been increasingly utilized for various benign and malignant hepatopancreatobiliary (HPB) indications[10-16]. After the adoption of laparoscopy in the 1990s, published literature comparing the minimally invasive approach to open surgery demonstrated improved outcomes such as shorter hospital length of stay (LOS), lower morbidity, improved cosmesis, and more rapid return to baseline functional status without compromising oncological outcomes. The robotic platform overcame some of the limitations of laparoscopy as it has the added benefit of three-dimensional visualization, stabilization of tremors, reduced operative fatigue, and improved ergonomics from the console-surgeon interface. Indocyanine Green (ICG) is a near-infrared spectrum fluorescence used in laparoscopic and robotic surgery that has been shown to be useful in delineating anatomical structures[17,18]. The dye is almost completely metabolized by the liver and excreted through the bile ducts, which is why it can be useful in technically-complex procedures such as the surgical resection of CC[17]. While well-described for hepatic and pancreatic resection, there was a paucity of reports on the use of the MIS approach in the treatment of CC. This is the first comprehensive review of laparoscopic and robotic assisted approaches for the surgical resection of choledochal cysts. Previous reviews have either compared only one approach[19] or have combined the results of previous literature focusing on only one aspect of the procedure[20]. Due to the technical complexity and steeper learning curve of minimally invasive biliary reconstruction, the MIS approach has not been as widely adopted in biliary surgery. We herein review the use of laparoscopic and robotic-assisted surgery in the treatment of CC.
METHODS
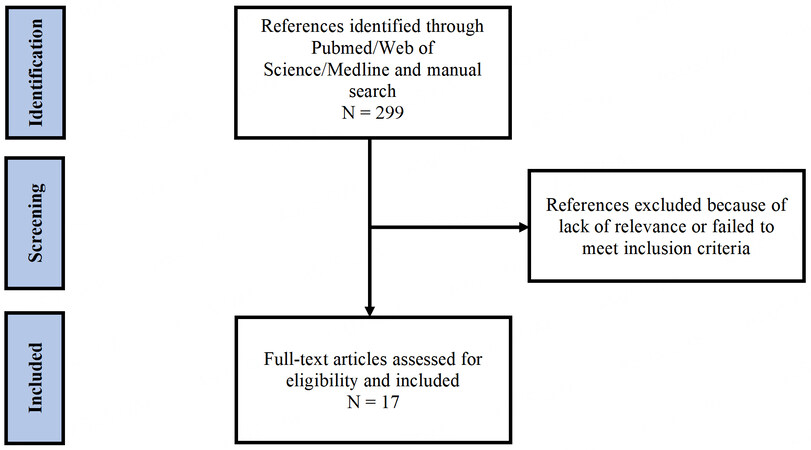
A comprehensive review of the literature was performed using MEDLINE/PubMed and Web of Science databases with a search end date of December 29, 2022. In PubMed, the terms “choledochal cyst”, “biliary cyst”, “robotic assisted”, “laparoscopic” and “minimally invasive surgery” were used. Articles published in English were assessed according to these eligibility criteria. Duplicate publications, single case reports, review articles and studies with no reported treatment were excluded. An expert review of the available literature was performed, and the most relevant and informative publications were identified for inclusion. Data were used to review the use of laparoscopic and robotic-assisted surgery in the treatment of CC [Figure 1].
Laparoscopic choledochal cyst resection
Background
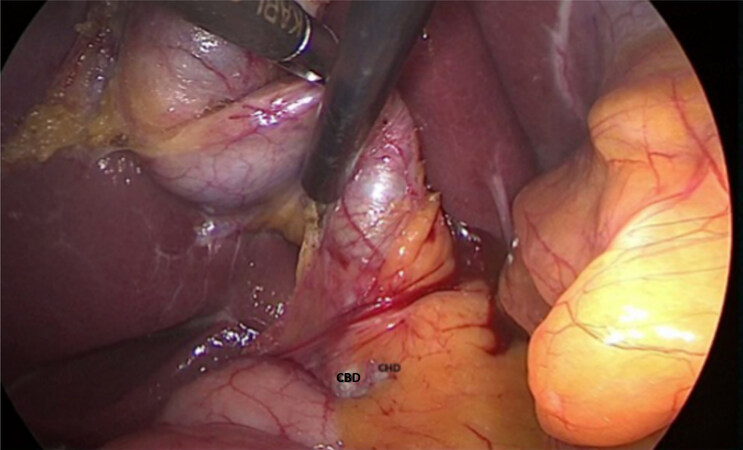
The first ever reported laparoscopic choledochal cyst resection (LCCR) was described by Farello and colleagues in 1995 with a successful hepatic-jejunal roux-en-y loop anastomosis in a six-year-old girl[21]. In subsequent years, the laparoscopic approach was progressively adopted and described by many surgeons and institutions to treat CC [Figure 2]. Laparoscopy has been repeatedly demonstrated to be safe and feasible for the treatment of CC. However, this approach is technically complex and therefore has a considerable learning curve.
Outcomes
Since first being described by Farello and colleagues, LCCR has been reported in numerous case series, case-control studies, and meta-analyses. In the early 2000s, single-center studies demonstrated the feasibility of the laparoscopic approach among adult patients with various types of CC[22-24]. In the last decade, larger case series demonstrating the safety and feasibility of LCCR were published[25-29]. Hwang and colleagues described their early experience in 20 patients with Type I and IV CC undergoing LCCR. Similar morbidity and mortality rates were noted among patients undergoing LCCR compared with historical data from patients in the literature who had undergone an open approach; however, LCCR was associated with longer operative times and high conversion rates, largely attributable to the learning curve given the technically challenging nature of the procedure[25]. Similarly, Jang and colleagues reported comparable short-term outcomes vs. the open approach while demonstrating better cosmetic and functional results[26]. In a separate study, Aly and colleagues compared using LCCR among patients undergoing surgical resection during two time periods (1996-2005 vs. 2006-2015). The authors noted improved operative outcomes among patients treated in the more recent time period with no conversions to open resection and only one case requiring hand assistance during laparoscopic resection; the improved operative outcomes were attributed to surgeon experience and improvement in surgical skills over time[29].
A more recent multi-institutional study by Margonis and colleagues utilized a propensity score matching analysis to compare patients with CC undergoing open CC resection (OCCR) vs. minimally invasive surgery (MIS), which included patients undergoing either laparoscopic or robotic-assisted surgery. After propensity-matching, the MIS approach was associated with decreased length-of-stay (LOS) (open: 7 days vs. MIS: 5 days), lower estimated blood loss (EBL) (open: 50 mL vs. MIS: 17.5 mL), yet longer operative times (open: 237 min vs. MIS: 301 min) compared with patients who underwent OCCR (all P < 0.05). Both patient cohorts had a similar incidence of postoperative morbidity and long-term overall survival[30]. The overall degree of complications did not differ between the OCCR (Clavien Dindo grades I-II, n = 13; grades III-IV, n = 15) and MIS cohorts (Clavien Dindo grades I-II, n = 5; grades III-IV, n = 5) (P = 0.85)[30]. Another study from a group in China demonstrated similar results with decreased LOS, decreased EBL, and higher operative times among patients undergoing LCCR vs. OCCR.[31] Of note, the accumulation of surgeon experience markedly decreased operative time (290 min in the early cohort vs. 198 min in the late cohort). A systematic review and meta-analysis that compared LCCR vs. OCCR among 1,408 patients (LCCR, n = 611 vs. OCCR, n = 797) in 7 studies demonstrated that LCCR was associated with shorter hospital LOS, earlier recovery of bowel function, lower rates of intraoperative blood transfusions, and a decreased relative risk for adhesive intestinal obstruction, yet longer operative times[19]. Moreover, the meta-analysis demonstrated no difference among patients in terms of the total number of postoperative complications, and biliary-specific complications such as bile leak, intra-abdominal bleeding, and pancreatitis. Overall, LCCR was associated with improved short-term outcomes; while the main disadvantage was longer operative times, this factor may be mitigated in the hands of experienced HPB surgeons [Table 1].
Published literature comparing laparoscopic choledochal cyst resections to open choledochal cyst resections
| Year | Author | Publication type | Choledochal cyst type | Sample size |
| 2001 | Tanaka et al.[22] | Retrospective | Unspecified | 8 (All L) |
| 2006 | Jang et al.[23] | Retrospective | Ia, Ic, IV | 12 (All L) |
| 2008 | Palanivelu et al.[24] | Retrospective | Ib, Iva | 35 (All L) |
| 2012 | Hwang et al.[25] | Retrospective | Ia, Ic, IVa | 20 (All L) |
| 2013 | Jang et al.[26] | Retrospective | Ia, Ib, Ic, II, III, IV | 82 (All L) |
| 2015 | Senthilnathan et al.[27] | Retrospective | I, IVa | 55 (All L) |
| 2015 | Duan et al.[28] | Retrospective | Ia, Ic | 31 (All L) |
| 2018 | Aly et al.[29] | Retrospective | Ia, IVa, IVb | 36 (All L) |
| 2015 | Margonis et al.[30] | Retrospective | I, II, III, IV | 368 (O: 332, MIS: 36) |
| 2014 | Liu et al.[31] | Retrospective | Ia, Ic, IVa | 74 (O: 39, L: 35) |
| 2015 | Zhen et al.[19] | Systematic review and meta-analysis | Unspecified | 1408 (O: 797, L: 611) |
Robotic choledochal cyst resection
Background
The robotic platform has been increasingly adopted as the laparoscopic approach has several limitations including three-dimensional visualization, limited range of instrument motion, and inferior surgeon ergonomics. With the technical complexity associated with the surgical resection of CC, the robotic platform may mitigate some of the technical difficulties encountered with rigid laparoscopic instruments and potentially result in shorter operative times. The robotic platform does, however, come with some limitations such as requirements to re-dock the robot in case the operation field is shifted or the risk of instrument collision in small surgical fields. The first robotic CC resection (RCCR) was described in a case report by Woo and colleagues in 2006[32]. Several case reports have since been published following Woo and colleagues’ initial description, which have demonstrated the widespread feasibility of the robotic approach based on data from larger case series comparing the robotic approach to LCCR and OCCR
Outcomes
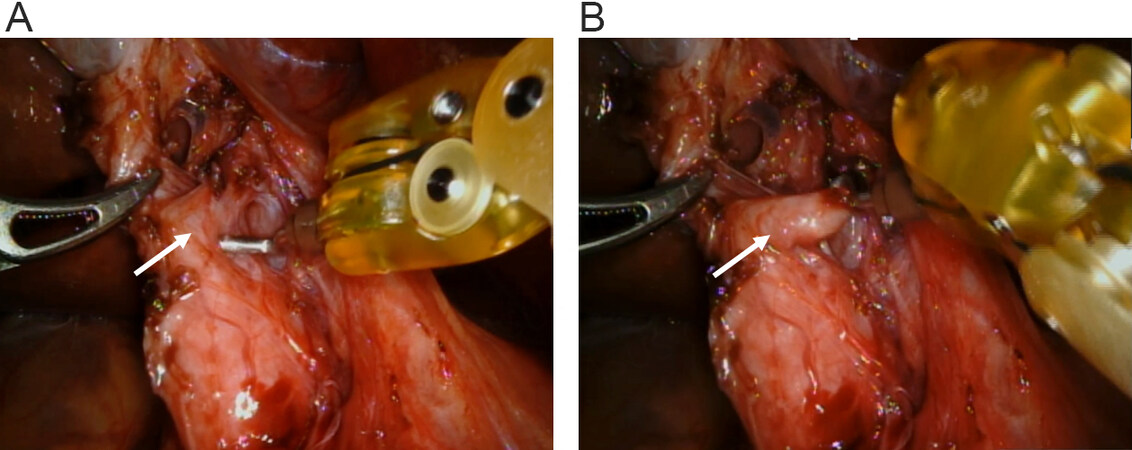
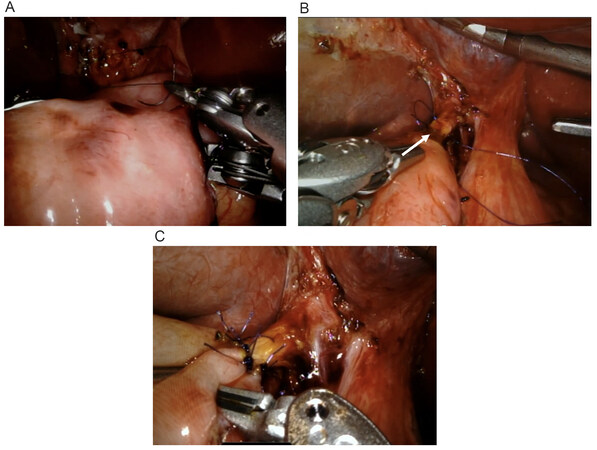
There are only a few published case series in the literature comparing RCCR to LCCR in adult patients. As noted, the study by Margonis and colleagues is the largest series to date that reported on short-term outcomes of patients undergoing robotic-assisted resection for CC[30]. More recently, Lee and colleagues described their experience utilizing a robotic-hybrid CC excision whereby patients underwent a laparoscopic dissection before the robotic platform was utilized for the hepaticojejunostomy (HJ) anastomosis[33]. The authors compared this technique to the laparoscopic-only approach and demonstrated that the robotic-assisted approach was associated with no short-term complications (22.4% vs. 0%; P = 0.029) such as bleeding, development of intra-abdominal fluid collections, bile leak, wound infections, and ileus. However, patients in the robotic cohort had longer operative times (247.94 ± 54.14 vs. 181.31 ± 43.06; P < 0.05), which the authors attributed to lengthy docking times and staff unfamiliarity with robotic instruments[33]. Similar to LCCR, there was a learning curve associated with the implementation of the robotic platform. The accumulation of surgeon experience resulted in an 80-min decrease in operative time over the course of the case series. In a similar study, Han and colleagues demonstrated the safety and feasibility of the robotic platform in adults with comparable short-term outcomes among patients in the RCCR and LCCR cohorts[34]. A more recent retrospective analysis by Yoon and colleagues demonstrated similar perioperative outcomes such as operative time, EBL, and postoperative complications among patients undergoing LCCR and RCCR[35]. The authors reported, however, a higher total hospital charge in the RCCR cohort ($6,568 ± 1,047 vs. $7,331 ± 720, P= 0.035). The $763 difference in cost was attributed to insurance reimbursement difficulties, as robotic surgery was not reimbursed by the National Health Insurance Corporation in South Korea. Of note, the cost for postoperative care in the study was higher in the LCCR group ($1,098 ± 260 vs. $716 ± 264, P = 0.001)[35]. The authors attributed the cost difference to an increase in the amount of routinely used drugs, combined with an increase in the volume of laparoscopic surgery over time. Morikawa and colleagues compared 36 patients undergoing open, laparoscopic, and robotic resections. Higher operative times were again associated with the MIS approach, yet there was shorter hospital LOS, lower EBL, and lower rates of internal stents. Among patients undergoing an MIS approach, the RCCR cohort had shorter operative times during the HJ anastomosis portion of the surgery compared to LCCR.
A systematic review and meta-analysis by Zhang and colleagues compared LCCR and RCCR among patients with type I through IV CC. Six studies (3 adult studies with a total of 162 patients) were included; patients treated with the robotic approach had a shorter hospital LOS but longer operative times. Estimated blood loss, as well as the incidence of bile leak, wound infection, postoperative bleeding, postoperative cholangitis, anastomotic strictures, adhesive intestinal obstructions, residual cysts, and incidence of biliary stones, were the same among patients treated with LCCR vs. RCCR[20]. Collectively, the data strongly suggest that the robotic platform may offer an advantage in the HJ anastomosis portion of CC resection [Figure 5] vs. laparoscopy while providing comparable short-term outcomes compared with the LCCR approach, yet better results than the OCCR approach with decreased EBL and shorter hospital LOS. The longer operative times associated with the robotic platform will likely be mitigated over time in the hands of experienced HPB surgeons [Table 2].
Figure 5. (A, B, and C) Robotic hepaticojejunostomy anastomosis (arrow) after choledochal cyst resection.
Published literature comparing robotic choledochal cyst resections to laparoscopic and open choledochal cyst resections
| Year | Author | Publication type | Choledochal cyst type | Sample size |
| 2015 | Margonis et al.[30] | Retrospective | I, II, III, IV | 368 (O: 332, MIS: 36) |
| 2018 | Lee et al.[33] | Retrospective | Ia, Ib, Ic, II, III, IVa, IVb | 67 (L: 49, R: 18) |
| 2018 | Han et al.[34] | Retrospective | Ia, Ib, Ic, IVa, IVb | 67 (L: 47, R: 22) |
| 2021 | Yoon et al.[35] | Retrospective | I, II | 39 (L: 23, R: 16) |
| 2022 | Morikawa et al.[36] | Retrospective | Ia, Ic, IVa | 36 (O: 16, L: 15, R: 5) |
| 2022 | Zhang et al.[20] | Systematic review and meta-analysis | Ia, Ib, Ic, II, III, IVa, IVb | 173 (L: 119, R: 56) |
Summary
Despite the technical complexity associated with minimally invasive HPB surgery related to CC resection, an increasing number of surgeons and hospitals have adopted these techniques. A minimally invasive approach to CC likely has improved perioperative outcomes with shorter LOS, return to baseline function, as well as improved cosmesis vs. OCCR. Longer operative times with minimally invasive approaches to CC have been attributed to steep learning curves, which have improved over time as surgeons become more facile with this technique. RCCR likely provides an additional advantage over LCCR due to more degrees of freedom with the instruments, providing a greater ability to perform the dissection and HJ reconstruction. In particular, the robotic platform overcomes some of the shortcomings associated with laparoscopic surgery and thus decreases operative times when constructing the HJ. It is important to note that there are several contraindications to the MIS approach including perforated cysts, pneumoperitoneum, inability to tolerate general anesthesia, hemodynamic instability, coagulopathy, and portal hypertension. It is also important to note that this study has several limitations including selection bias and a relatively small sample size.
CONCLUSION
Both LCCR and RCCR have demonstrated similar rates of long-term postoperative complications and overall survival when compared to OCCR. Overall, a minimally invasive approach to surgical management of CC should be strongly considered. Future prospective randomized studies should compare both minimally invasive approaches to the open approach to assess short- and long-term complications associated with each surgical platform. Selection criteria for patients undergoing MIS for CC resection will also need to be defined better as experience with this approach expands.
DECLARATIONS
Authors’ contributionsMade substantial contributions to the conception and design of the study and performed data analysis and interpretation: Hamad A, Nathan JD, Pawlik TM
Performed data acquisition, as well as providing administrative, technical, and material support: Hamad A, Nathan JD, Pawlik TM
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2023.
REFERENCES
1. Wiseman K, Buczkowski AK, Chung SW, Francoeur J, Schaeffer D, Scudamore CH. Epidemiology, presentation, diagnosis, and outcomes of choledochal cysts in adults in an urban environment. Am J Surg 2005;189:527-31; discussion 531.
2. Alonso-Lej F, Rever WBJ, Pessagno DJ. Congenital choledochal cyst, with a report of 2, and an analysis of 94, cases. Int Abstr Surg 1959;108:1-30.
3. Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: Classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg 1977;134:263-9.
4. Todani T, Watanabe Y, Toki A, Morotomi Y. Classification of congenital biliary cystic disease: special reference to type Ic and IVA cysts with primary ductal stricture. J Hepatobiliary Pancreat Surg 2003;10:340-4.
5. Todani T. Congenital choledochal dilatation: classification, clinical features, and long-term results. J Hepatobiliary Pancreat Surg 1997;4:276-82.
6. Umar J, Kudaravalli P, John S. Caroli disease. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513307/ [Last accessed on 26 Apr 2023].
8. Xia HT, Dong JH, Yang T, Zeng JP, Liang B. Extrahepatic cyst excision and partial hepatectomy for Todani type IV-A cysts. Dig Liver Dis 2014;46:1025-30.
10. Ejaz A, Sachs T, He J, et al. A comparison of open and minimally invasive surgery for hepatic and pancreatic resections using the Nationwide Inpatient Sample. Surgery 2014;156:538-47.
11. Jin T, Altaf K, Xiong JJ, et al. A systematic review and meta-analysis of studies comparing laparoscopic and open distal pancreatectomy. HPB 2012;14:711-24.
12. Lin NC, Nitta H, Wakabayashi G. Laparoscopic major hepatectomy: a systematic literature review and comparison of 3 techniques. Ann Surg 2013;257:205-13.
13. Hamad A, Zenati MS, Nguyen TK, Hogg ME, Zeh HJ 3rd, Zureikat AH. Safety and feasibility of the robotic platform in the management of surgical sequelae of chronic pancreatitis. Surg Endosc 2018;32:1056-65.
14. Girgis MD, Zenati MS, King JC, et al. Oncologic outcomes after robotic pancreatic resections are not inferior to open surgery. Ann Surg 2021;274:e262-8.
15. Zureikat AH, Moser AJ, Boone BA, Bartlett DL, Zenati M, Zeh HJ 3rd. 250 robotic pancreatic resections: safety and feasibility. Ann Surg 2013;258:554-9; discussion 559.
17. Boni L, David G, Mangano A, et al. Clinical applications of indocyanine green (ICG) enhanced fluorescence in laparoscopic surgery. Surg Endosc 2015;29:2046-55.
18. Autorino R, Zargar H, White WM, et al. Current applications of near-infrared fluorescence imaging in robotic urologic surgery: a systematic review and critical analysis of the literature. Urology 2014;84:751-9.
19. Zhen C, Xia Z, Long L, et al. Laparoscopic excision versus open excision for the treatment of choledochal cysts: a systematic review and meta-analysis. Int Surg 2015;100:115-22.
20. Zhang K, Zhao D, Xie X, Wang W, Xiang B. Laparoscopic surgery versus robot-assisted surgery for choledochal cyst excision: a systematic review and meta-analysis. Front Pediatr 2022;10:987789.
21. Farello GA, Cerofolini A, Rebonato M, Bergamaschi G, Ferrari C, Chiappetta A. Congenital choledochal cyst: video-guided laparoscopic treatment. Surg Laparosc Endosc 1995;5:354-8.
22. Tanaka M, Shimizu S, Mizumoto K, et al. Laparoscopically assisted resection of choledochal cyst and Roux-en-Y reconstruction. Surg Endosc 2001;15:545-52.
23. Jang JY, Kim SW, Han HS, Yoon YS, Han SS, Park YH. Totally laparoscopic management of choledochal cysts using a four-hole method. Surg Endosc 2006;20:1762-5.
24. Palanivelu C, Rangarajan M, Parthasarathi R, Amar V, Senthilnathan P. Laparoscopic management of choledochal cysts: technique and outcomes--a retrospective study of 35 patients from a tertiary center. J Am Coll Surg 2008;207:839-46.
25. Hwang DW, Lee JH, Lee SY, et al. Early experience of laparoscopic complete en bloc excision for choledochal cysts in adults. Surg Endosc 2012;26:3324-9.
26. Jang JY, Yoon YS, Kang MJ, et al. Laparoscopic excision of a choledochal cyst in 82 consecutive patients. Surg Endosc 2013;27:1648-52.
27. Senthilnathan P, Patel ND, Nair AS, Nalankilli VP, Vijay A, Palanivelu C. Laparoscopic management of choledochal cyst-technical modifications and outcome analysis. World J Surg 2015;39:2550-6.
28. Duan X, Mao X, Jiang B, Wu J. Totally laparoscopic cyst excision and Roux-en-Y hepaticojejunostomy for choledochal cyst in adults: a single-institute experience of 5 years. Surg Laparosc Endosc Percutan Tech 2015;25:e65-8.
29. Aly MYF, Mori Y, Miyasaka Y, et al. Laparoscopic surgery for congenital biliary dilatation: a single-institution experience. Surg Today 2018;48:44-50.
30. Margonis GA, Spolverato G, Kim Y, et al. Minimally invasive resection of choledochal cyst: a feasible and safe surgical option. J Gastrointest Surg 2015;19:858-65.
31. Liu Y, Yao X, Li S, Liu W, Liu L, Liu J. Comparison of therapeutic effects of laparoscopic and open operation for congenital choledochal cysts in adults. Gastroenterol Res Pract 2014;2014:670260.
32. Woo R, Le D, Albanese CT, Kim SS. Robot-assisted laparoscopic resection of a type I choledochal cyst in a child. J Laparoendosc Adv Surg Tech A 2006;16:179-83.
33. Lee H, Kwon W, Han Y, Kim JR, Kim SW, Jang JY. Comparison of surgical outcomes of intracorporeal hepaticojejunostomy in the excision of choledochal cysts using laparoscopic versus robot techniques. Ann Surg Treat Res 2018;94:190-5.
34. Han JH, Lee JH, Hwang DW, et al. Robot resection of a choledochal cyst with Roux-en-y hepaticojejunostomy in adults: Initial experiences with 22 cases and a comparison with laparoscopic approaches. Ann Hepatobiliary Pancreat Surg 2018;22:359-66.
35. Yoon JH, Hwang HK, Lee WJ, Kang CM. Minimally invasive surgery for choledochal cysts: Laparoscopic versus robotic approaches. Ann Hepatobiliary Pancreat Surg 2021;25:71-7.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Hamad A, Nathan JD, Pawlik TM. Laparoscopic and robotic approaches for treatment of choledochal cysts in adults. Mini-invasive Surg 2023;7:16. http://dx.doi.org/10.20517/2574-1225.2023.03
AMA Style
Hamad A, Nathan JD, Pawlik TM. Laparoscopic and robotic approaches for treatment of choledochal cysts in adults. Mini-invasive Surgery. 2023; 7: 16. http://dx.doi.org/10.20517/2574-1225.2023.03
Chicago/Turabian Style
Hamad, Ahmad, Jaimie D. Nathan, Timothy M. Pawlik. 2023. "Laparoscopic and robotic approaches for treatment of choledochal cysts in adults" Mini-invasive Surgery. 7: 16. http://dx.doi.org/10.20517/2574-1225.2023.03
ACS Style
Hamad, A.; Nathan JD.; Pawlik TM. Laparoscopic and robotic approaches for treatment of choledochal cysts in adults. Mini-invasive. Surg. 2023, 7, 16. http://dx.doi.org/10.20517/2574-1225.2023.03
About This Article
Special Issue
Copyright
Data & Comments
Data

 Cite This Article 8 clicks
Cite This Article 8 clicks












Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.